INTRODUCTION
Endodontic therapy consists of the preparation of the main root canal to achieve disinfection of the canal system, ending with a hermetic and three-dimensional sealing.1 Before final sealing, the antibacterial phase of the treatment within the canal system must be completed with adequate mechanical preparation and abundant irrigation using effective solutions against the microorganisms inside the canal. Once this state of asepsis is completed, recontamination should be avoided.2 The sealing is made with inert antibacterial materials that promote a stable sealing, prevent the entry of microorganisms of the oral cavity or peri radicular tissues, and stimulate the repair process.3
According to Maisto and Lasala, the endodontic materials used for root canal sealing can be classified according to the state in which they are presented:3
The most common endodontic sealing technique is based on the use of guttapercha semisolid cones as the base material; however, guttapercha alone is not sufficient to produce sealing, and needs to be supplemented with an endodontic cement.4 Ideally, the sealant should be able to create an effective bonding between the base material and the root dentin avoiding microleakage, it should not be toxic and should promote periapical healing.5,6
Epoxy resin-based sealants were introduced in endodontics by Schroeder,7 and are currently widely used for root canal sealing procedures thanks to their favorable behavior, such as good adherence to the tooth structure, adequate working time, easy handling, and good sealing.8,9
One of the most widely used brands is Topseal® (Dentsply Maillefer, Switzerland), an endodontic sealant based on epoxydinomine resin, which contains calcium tungsten, zirconium oxide, iron, aerosil and silicone oil, and calcium hydroxide. It has low solubility, adequate radiopacity, adhesion to root dentin, antimicrobial activity and adequate biological properties.10 This cement has been extensively evaluated for its physicochemical characteristics and biological response, showing excellent flow rate, sealing and low solubility properties.11,12 Thanks to these properties it can be considered as the gold standard.
A new brand of an epoxy resin-based sealant has recently been introduced to the Colombian market, known as AdSeal™ (Meta, Biomed, Cheongju, South Korea). According to the manufacturer, this sealant contains bismuth phosphate, zinc oxide and calcium phosphate mixed with vinyl polymer. It is available in two tubes containing the paste.8 This endodontic sealant has few reports in the literature concerning its biological behavior and physicochemical properties.8,9 In 2011, Martian et al found out that epoxy resin-based sealing cements AH Plus, Acroseal, and AdSeal™ have similar adaptation to the root canal, solubility, flow rate and film thickness, with statistically significant differences for radiopacity and setting time.13
The requirements established by the Colombian Technical Standard NTC 4390 (root canal filling materials), an identical standard translated from ISO 6876:2012, include radiopacity equal to or less than 3 mm of aluminum, solubility lower than 3%, flow rate not lower than 17 mm, film thickness lower than 50 µm, and a setting time not exceeding 10% of the time specified by the manufacturer.14,15 The Topseal® cement satisfactorily meets the requirements of this standard.13,25
Not all materials available for root canals sealing strictly comply with this standard, it is therefore very important to study the physicochemical properties of commercially available endodontic cements. This paper aims to analyze some properties of the AdSeal™ endodontic sealant, in order to help endodontists select the right materials for a successful clinical practice.
METHODS
The study was evaluated and approved by the Ethics and Research Methodology Committee of the Universidad de Antioquia, School of Dentistry, on 18 December 2015, minutes 20-15.
A comparative in vitro study was conducted to evaluate the radiopacity, flow rate, and film thickness of epoxy resin-based sealants Topseal® and AdSeal™ using the criteria specified by the ISO 6876:2012 and NTC 4390 standards.14,15
Radiopacity
Ten acrylic molds measuring 10 mm in diameter by 1 mm tick were filled with AdSeal™ and Topseal® to obtain 5 samples of each sealant. The discs were stored at 37 oC and 100% humidity until final setting.
Five discs of the same sealant were grouped on a digital phosphor plate sensor (Carestream CS 7600) along with the stepped aluminum block. X-rays were taken using a Gendex Gx 770 equipment (70 KV-7mA) at a focal length of 30 mm 4 times for each sealant, with exposure time of 0.5 sec (Figure 1).
Figure 1
Digital images of sealant discs and aluminum block. A. Topseal® and B. AdSeal™.
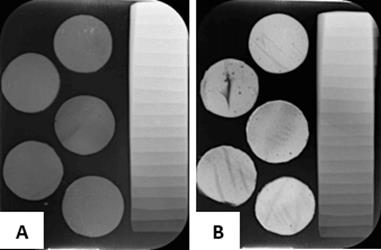
Source: by the authors
The images were analyzed on the ImageJ software16 to determine the gray shade of the discs for each sealant, in search of their equivalence in mm in the Al block.
Flow rate
Using an insulin syringe, 0.05 ml of each sealant were placed on a 40 x 40 mm glass plate. 180 ± 5 sec after initiating the mixture, another glass plate of the same size 40 x 40mm x 20 g was placed on the sealant, adding and additional weight of 100 g. 10 minutes after starting the mixture, the weight was removed, measuring the diameter reached by each cement in two sites, maximum and minimum (Figure 2). These cement discs were photographed, and the images analyzed with the help of the ImageJ software. This procedure was repeated 5 times for each cement (5 Topseal® and 5 AdSeal™).
Film Thickness
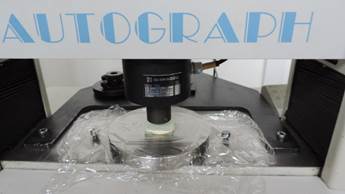
A sufficient amount of cement was prepared to cover an area of 4 x 4 cm. Another equal glass plate was placed on the sealant. 180 ± 10 sec. of starting the mixture, the assembly of the two plates with the sealant was brought to the universal testing machine (AGIS 5KN), applying a compressive vertical load of 150 N (Figure 3). 10 min after starting the mixture, the load was removed and the thickness of the assembly (glass and cement plates) was measured with the help of the stereomicroscope at three equidistant points, recording the average measurements (Figure 4). This procedure was repeated 5 times for each cement (5 Topseal® and 5 AdSeal™).
RESULTS
Radiopacity
A data normality test was performed using the Shapiro Wilk Test, finding out a non-normal distribution with a p value of 0.009415. For this reason, nonparametric tests were conducted to determine the aluminum level of data from both AdSeal™ and Topseal®.
The Wilcoxon’s nonparametric test was used, as it helps compare the median of two related samples and determine if there are differences between them.
The radiopacity values of the AdSeal™ cement were 2.4 mm of Al, while those of the Topseal® cement were 9.6 mm Al, with statistically significant difference in terms of the sealants’ radiopacity (p < 0.05).
Flow rate
A data normality test was performed using the Shapiro Wilk Test, finding out a normal distribution (p = 0.3436); therefore, parametric tests were used to determine whether there is a statistically significant difference between the flow rate data of the two sealants.
A parametric variance analysis test was performed, showing a statistically significant difference between the flow rate data of AdSeal™ and Topseal®, with a p value of 0.0001863. In addition, a Tukey’s HSD test was performed to compare the flow rate data of AdSeal™ and Topseal®, yielding a significance level of 1%, thus confirming the presence of statistically significant differences (p value = 0.0001863).
The flow rate values of the AdSeal™ and Top-seal® sealants averaged 27.89 mm and 19.72 mm respectively, showing that the flow rate of AdSeal™ is 8 mm greater than that of Top-seal®.
Film Thickness
The data were analyzed with the Shapiro Wilk test, finding out normal distribution (p = 0.6382). A parametric variance analysis test was applied, showing no statistically significant difference between the film thickness data (p = 0.4927).
The AdSeal™ and Topseal® sealants have an average film thickness of 0.083 mm and 0.062 mm respectively.
DISCUSSION
There was a statistically significant difference in the radiopacity of AdSeal™ and Topseal® sealants with values of 9.6 mm and 2.4 mm respectively, favoring Topseal®. Sealing cements radiopacity may vary due to precipitation of radiopacity agents at the lower end of the container tube, while the top part may have a smaller amount of such agents.13 This is why to create the test samples in this study, the total amount of the containing material was dispensed, mixing evenly once to avoid disparities in the radiopacity agents.
In this study, images were obtained on phosphor plates, digitized on a CS 7600 Carestream scanning equipment and analyzed using the ImageJ software, which differs from conventional X-rays that rely on chemical processes like revealing and fixing. In addition, the analysis with conventional films is usually performed on a densitometer, which only covers a small area of the image, while digital images offer a software that enables analysis in wider areas, and therefore the collected data can be more representative of both the sealing disc and the aluminum wedge.
ISO 6876:2012 states that root canal filling materials must have a radiopacity of ≥ 3 mm of aluminium.15 In the present study, the radiopacity of Topseal® was 9.6 mm of Al, which is consistent with the studies by Tagger and Katz 2003,19 Tanomaru-Filho 2007,20 and Gümrü 2013;21 however, AdSeal™ yielded 2.4 mm of Al, which is below the minimum requirement established by the standard. The difference in radiopacity between the sealants tested in this study was 6 mm of Al, agreeing with the studies by Marciano 2003,13 Gümrü 2013,21 Taşdemir 2008,22 and Ehsani 2013,23 who found differences greater than 7 mm between AdSeal™ and AH plus.
Discs measuring 10 x 1 mm were created for the radiopacity analysis, obtaining X-ray images after the sealant was forged, unlike other studies such as those by Taşdemir 2008,22 Gümrü 2013,21 and Ehsani 2013,23 where X-rays were taken immediately after preparing the material, resulting in higher radiopacity values than ours; perhaps the newly mixed sealant reflects greater radiopacity than it does right after setting time.
Proper flow is an important feature for a root canal sealant to fill spaces between the gutta-percha cone and the dentinal wall. However, excessive flow increases the risk of extrusion from sealant to periodontal tissue.24
ISO 6876:2012 states that, when flow rate is determined according to numeral 5.2, each disc should have a diameter of no less than 17 mm.15 In this study, AdSeal™ and Topseal® yielded diameters of 27.89 mm and 19.72 mm respectively, both satisfactory results according to the standard.
The present study found out that AdSeal™ has more fluidly than Topseal® with statistically significant differences, agreeing with the study by Song et al in 2016.25 However, Marciano et al in 201113 found no significant differences in flow rate values between AH plus and AdSeal™.
ISO 6876:2012 states that sealants must have a film thickness of no more than 50 µm when tested according to numeral 5.5.15 In our study, AdSeal™ and Topseal® had a film thickness of 83 mm and 62 mm respectively on average, both with higher values, but unlike the standard, which recommends using a micrometer as a measuring instrument, we used stereomicroscope image analysis as a measuring instrument, which in theory provides greater accuracy than a micrometer.
We found out that AdSeal™ has a film thickness of 21 µm greater than Topseal®, but this difference is not statistically significant (p = 0.4927), agreeing with Marciano et al, who in 2011 found out that the results regarding the film thickness of the evaluated sealants showed a difference of 21.5 µm between AdSeal™ and AH Plus without being statistically significant.13
One limitation of this study was sample size, which explains the non-normal distribution of the variable and the need for nonparametric statistics.
CONCLUSIONS
The tested cements showed statistically significant differences in radiopacity and flow rate, with Topseal® being the one with the highest radiopacity and AdSeal™ with the most flow rate, while film thickness showed no significant statistical differences.
The methodology used in this study to measure film thickness yielded higher results than allowed by ISO 6876:2012; we then recommend this method to be complemented by the conventional measurement technique with a micrometer for more reliable results.
For radiopacity analysis, new studies are recommended measuring radiopacity on freshly prepared material and after setting time. We also recommend applying the entire sealing material container tube into the mixture to ensure that the radiopacity agents of each material are fully incorporated.
It is necessary to continue studying the physical, chemical and mechanical characteristics of these cements in order to increase their reliability and use in clinical endodontic practice.
It is also recommended to carry out new studies with larger samples, in order to achieve conclusions based on parametric statistics.