INTRODUCTION
Temporomandibular disorders (TMDs) present orofacial symptoms such as pain, masticatory dysfunction, difficulty in opening the mouth, limited jaw movements and chronic inflammation of the temporomandibular joint (TMJ).1 Pain is the main symptom affecting the functioning of the masticatory system and is therefore recognized as a major source of disability that affects quality of life.2
In terms of TMD symptom relief, the literature discusses various clinical procedures, such as the use of occlusal splints, physical therapy and low-level laser therapy (LLLT). It is important for these actions to be supported by clinical evidence regarding their scientific benefits and efficacy.3,4
LLLT is one of the most used therapies today to treat symptoms such as inflammation and pain in TMDs. However, LLLT is not effective in the treatment of the disorder per se.2,5 Due to their analgesic and anti-inflammatory effects, various types of lasers, such as helium-neon (HeNe) and arsenidegallium-aluminum (GaAlAs), are used in the management of TMDs, with each being used at different wavelengths.1,6,7 The treatment is considered non-invasive, fast and safe.8
The literature describes favorable results in many clinical trials using LLLT for the treatment of signs and symptoms such as pain and trismus, but there is no specifically established protocol in terms of energy intensity, power, exposure time and number of applications.8-11
Below we present a systematic literature review to establish whether there is evidence that LLLT can reduce the main symptoms of TMDs and to determine the most effective application protocol.
METHODS
This systematic review was performed according to Preferred Reporting Items for Systematic Review and Meta Analyses (PRISMA).12 It was recorded in the International Prospective Register of Systematic Review PROSPERO (CRD42017076612).
Focal issue
The PICO issue was as follows: whether there is evidence of an efficient protocol for the use of LLLT for TMD symptom relief.
Search strategy
Two independent researchers (KVR and GLT) conducted a search in the principal data portals, PubMed, Scopus and Web of Science, considering specific outcomes of TMD symptoms such as pain, mouth opening and jaw movements, treated using different LLLT protocols, until September 30, 2017, and considering the following keywords: ((temporomandibular joint) OR tmj disorder)) OR tmj disfunction)) AND laser therapy) OR low level laser therapy)) OR photobiomodulation)) AND oral facial pain.
Inclusion and exclusion criteria
Only articles written in English and that met the following eligibility criteria were included: a) randomized clinical trials; b) studies specifying the type of laser used, including comparison groups with other laser types, other treatments, or placebo; and c) those presenting outcomes such as pain, mouth opening and jaw movements. Duplicate studies were removed using tools from EndNote version 2.5.0. Studies without a control group or an abstract, those evaluating diseases other than TMJ and animal studies were excluded.
Data extraction
After reading the titles and abstracts, two independent reviewers (KVR and GLT) selected the articles to be included. Disagreements between reviewers were resolved by consensus after discussion and evaluation by a third investigator (MCZD).
Articles meeting the inclusion criteria were read in full for data extraction onto an individualized form that included the type and place of study; age and sex of participants; qualification of the control or comparison group; type, power and length of laser wave; number of sessions; evaluation and results of the outcomes, and follow-up period.
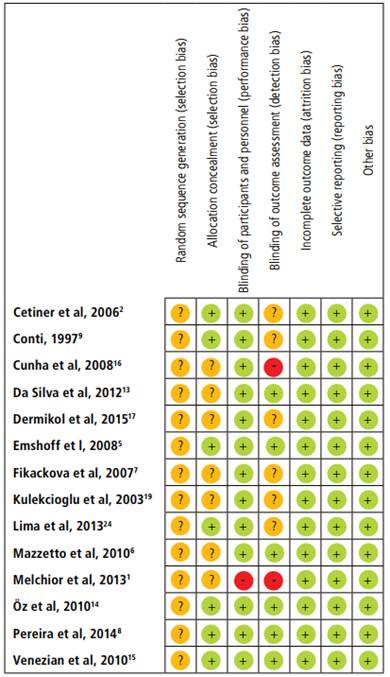
Bias evaluation
After data extraction, the studies were evaluated for biases using RevMan software 5.3 (Review Manager Computer program Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014), taking the following aspects into account: form of randomization and allocation of participants into experimental and control groups; whether there was blinding of participants and/or examiners; and whether there were any conflicts of interest.
RESULTS
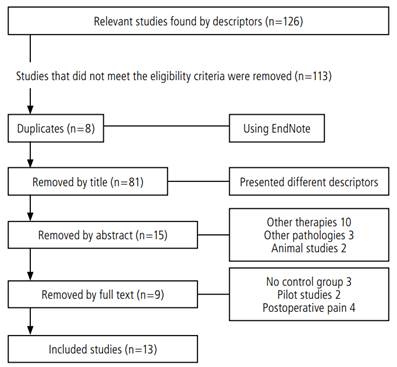
A total of 126 articles were initially retrieved. Eight duplicate studies were removed, along with 113 studies that did not meet the eligibility criteria. Figure 1 shows the flowchart for the search and exclusion of articles.
The characteristics of each selected study are shown in Table 1.
Table 1
Characteristics of each selected study
| Author, year | Study type | Participants | Laser Group I | Laser Group II | Control Group | Comparison intervention | Laser dosage | Number of sessions | Control | Follow-up (weeks) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cetiner et al, 20062 | Rand., pros., double blind | 39 | 24 | 15 | NA | GaAlAs - 830 nm, 7 J/cm2, 162 s | 10 | A, disconnected | 4 | ||
| Conti, 19979 | Rand., pros., double blind | 20 | 10 | 10 | NA | GaAlAs - 830 nm, 100 mW, 4 J/cm2, 40 s | 3 | A, disconnected | 3 | ||
| Da Cunha et al, 200816 | Rand., pros., double blind | 40 | 20 | 20 | NA | GaAlAs - 830 nm, 500 mW, 4 J/cm2, 20 s | 4 | A, disconnected | 4 | ||
| Da Silva et al, 201213 | Rand., pros., double blind, parall. | 45 | 15 | 15 | 15 | GaAlAs - 830 nm, 70 mW, 105 J/cm2 | GaAlAs - 830 nm, 70 mW, 52.5 J/cm2 | 10 | A, disconnected | 5 | |
| Demirkol et al, 201517 | Rand., pros., double blind, parall. | 30 | 10 | 10 | 10 | Occlusal splints | Nd:Yang - 1064 nm, 250 mW, 8 J/cm2, 20 s | 10 | NA | 3 | |
| Emshoff et al, 20085 | Rand., pros., double blind | 52 | 26 | 26 | NA | HeNe - 632.8 nm, 30 mW, 1.5 J/cm2 | 20 | A, disconnected | 8 | ||
| Fikácková et al, 20077 | Rand., pros., double blind, parall. | 80 | 33 | 28 | 19 | GaAlAs - 830 mm, 400 mW, 15 J/cm2 | GaAlAs - 830 mm, 400 mW, | 10 J/cm2 10 | A, disconnected | 4 | |
| Kulekcioglu et al, 200319 | Rand., pros., double blind | 35 | 20 | 15 | NA | GaAs - 904 nm, 17 mW, 3 J/cm2, 180 s | 15 | A, disconnected | 4 | ||
| Lima et al, 201324 | Rand., pros., double blind | 58 | 32 | 26 | NA | GaAlAs - 830 nm, 40 mW, 8 J/cm2, 60 s | 12 | A, disconnected | 6 | ||
| Mazzetto et al, 20106 | Rand., pros., double blind | 40 | 20 | 20 | NA | GaAlAs - 830 nm, 40 mW, 5 J/cm2, 50 s | 8 | A, disconnected | 4 | ||
| Öz et al, 201014 | Rand., pros., double blind, parall. | 40 | 20 | 20 | Occlusal splints | GaAlAs - 820 nm, 300 mW, 3 J/cm2, 10 s | 10 | 30-90 days | 5 | ||
| Pereira et al, 20148 | Rand., pros., double blind parall. | 19 | 19 side face | 19 side face | GaAlAs - 795 nm,100 mW, 8 J/cm2, infra red, 40 s | GaAlAs - 660 nm, 100 mW, 4 J/cm2 in TMJ, red 40 s | 3 | NA | 3 | ||
| Venezian et al, 201015 | Rand., pros., double blind, parall. | 48 | 24 | 24 | GaAlAs - 780 nm, 60 mW, 60 J/cm2, 40 s | GaAlAs - 780 nm, 50 mW, 25 J/cm2, 20 s | 8 | NA | 4 |
Figure 2 shows the risk of bias of each selected study.
The main outcomes of each study are shown in Table 2.
Table 2
main outcomes of each study
| Author, year | Pain | Mouth opening | |||||
|---|---|---|---|---|---|---|---|
| Experimental | Control | Comparison | Experimental | Control | Comparison | ||
| Cetiner et al, 20062 | Before | 7.56 (+ 1.46) | 6.57 (+1.91) | NA | 33.96 ± 8.35 | 35.83 ± 8.66 | NA |
| Immediately | 2.25 (+ 2.05) | 5.60 (+1.76) | NA | 39.67 ± 6.45 | 38.67 ± 8.37 | NA | |
| 4 weeks | 0.82 (+1.33) | 5.19 (+ 2.01) | NA | 40.96 ± 5.94 | 38.58 ± 8.42 | NA | |
| Conti, 19979 | Before | 56 | 44 | NA | 0.561 | 0.024 | NA |
| 3 weeks | 20 | 46 | NA | 0.035 | 0.098 | NA | |
| Cunha et al, 200816 | Before | 6.87 (+ 2.12) | NA | ||||
| 4 weeks | 3.62 (+ 2.45) | NA | |||||
| Da Silva et al, 201213 | Outset | 32.0 (+ 5.20) | 31.90 (+ 4.40) | 32.30 (+ 4.70) | |||
| Immediately | 32.93 (+ 5.51) | 32.27 (+ 4.67) | 34.73 (+ 5.35) | ||||
| 5 applications | 34.33 (+ 4.94) | 31.87 (+ 4.54) | 36.87 (+ 4.30) | ||||
| 10 applications | 37.20 (+ 4.81) | 31.53 (+ 4.11) | 36.87 (+ 4.22) | ||||
| 5 weeks | 35.80 (+ 4.98) | 30.87 (+ 4.11) | 34.80 (+ 4.42) | ||||
| Demirkol et al, 201517 | Before | 6.45 (+ 1.707) | 6.60 (+ 1.506) | 7.40 (+ 2.459) | |||
| 3 weeks | 1.50 (+ 2.273) | 2.0 (+ 2.39) | 6.60 (+ 2.319) | ||||
| Emshoff et al, 20085 | Before | 38.2 (+7.6) | 39.7 (+12.2) | NA | |||
| 2 weeks | 27.4 (+17.5) | 25.2 (+12.7) | NA | ||||
| 4 weeks | 20.9 (+17.7) | 16.5 (+15.0) | NA | ||||
| 8 weeks | 12.3 (+16.1) | 11.8 (+16.8) | NA | ||||
| Fikácková et al, 20077 | Worsening acute pain | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Worsening chronic pain | 1 (4%) | 0 (0%) | 1 (6%) | ||||
| Unchanged acute pain | 1 (11%) | 4(34%) | 3 (30%) | ||||
| Unchanged chronic pain | 3 (12%) | 8 (100%) | 5 (28%) | ||||
| Improved acute pain | 8 (89%) | 7 (66%) | 7 (70%) | ||||
| Improved chronic pain | 20 (84%) | 0 (0%) | 12 (67%) | ||||
| Kulekcioglu et al, 200319 | Before | 42.88 (+27.0) | 35.3 (+29.0) | NA | 36.0 (+8.0) | 37.4 (+11.2) | NA |
| Immediately | 10.5 (+8.4) | 8.0 (+9.4) | NA | 42. (+8.4) | 40.8 (+8.9) | NA | |
| 4 weeks | 5.5 (+17.9) | 5.3 (+6.4) | NA | 43.7 (+7.4) | 40.8 (+8.9) | NA | |
| Lima et al, 201324 | Without acute pain 1 | 0 | 34.4 | NA | 0 | 0 | NA |
| Without chronic pain | 0 | 0 | NA | 19.2 | 19.2 | NA | |
| Acute mild pain 1 | 0 | 65.6 | NA | 18.8 | 3.1 | NA | |
| Chronic mild pain | 0 | 7.7 | NA | 53.8 | 30.8 | NA | |
| Acute moderate pain 2 | 53.1 | 0 | NA | 81.3 | 46.9 | NA | |
| Chronic moderate pain | 7.7 | 76.9 | NA | 26.9 | 34.5 | NA | |
| Severe acute pain 2 | 43.8 | 0 | NA | 0 | 50 | NA | |
| Severe chronic pain | 50 | 15.4 | NA | 0 | 15.4 | NA | |
| Severe acute pain 2 | 3.1 | 0 | NA | NA | |||
| Severe chronic pain 3 | 42.3 | 0 | NA | NA | |||
| Mazzetto et al,20106 | Before | 5.40 | 5.80 | NA | 48.25 | 47.90 | NA |
| 8 applications | 2.10 | 4.45 | NA | 50.60 | 47.30 | NA | |
| 7 days | 2.50 | 5.15 | NA | 50.25 | 47.5 | NA | |
| 4 weeks | 2.95 | 5.60 | NA | 50.55 | 46.35 | NA | |
| Öz et al, 201014 | Before | 48.5 | NA | 52.7 | 44.20 (6.14) | 43.20 (6.57) | |
| 5 weeks | 16.8 | NA | 31.6 | 47.20 (5.51) | 44.45 (5.90) | ||
| Pereira et al, 20148 | Outset | 7.38 (1.7) | NA | 6.91 (1.6) | |||
| 24 hours | 5.04 (2.4) | NA | 4.65 (2.5) | ||||
| 30 days | 4.76 (2.8) | NA | 4.20 (2.4) | ||||
| 90 days | 4.84 (2.9) | NA | 4.44 (2.5) | ||||
| 180 days | 4.95 (2.9) | NA | 3.73 (2.6) | ||||
| Venezian et al, 201015 | Before | 7.66 | NA | 6.49 | |||
| Immediately | 4.87 | NA | 3.45 | ||||
| 4 weeks | 5.37 | NA | 4.12 | ||||
| Before | 7.99 | NA | 7.37 | ||||
| Immediately | 4.8 | NA | 3.87 | ||||
| 4 weeks | 5.45 | NA | 3.87 |
The laser type most commonly used was GaAlAg.2,6,8,9,13-15 The wavelength ranged from 830 nm to 904 nm, and the number of sessions ranged from 4 to 15. The energy density used ranged from 1.5 J/cm² 5 to 52.5 J/cm².13
An energy density of 3 J/cm2 was used by some authors (Kulekcioglu 200319, Ficácková 20077 and Öz 201014) in their clinical trials, with decreased pain in the groups treated by laser. Most authors used energy densities of 4 J/cm² and 8 J/cm2,2,8,9,11,16,17 with favorable results in terms of improvement in TMD symptoms.
Not all studies evaluated mouth opening.2,9,18 Cetiner 20062 evaluated masticatory difficulty as the outcome and, using an adapted visual analog scale (VAS), found an improvement in the group that used LLLT.
Regarding the evaluation of pain in the muscle insertion points made by operator palpation, in some studies, groups treated with lasers showed an improvement in pain of up to 4 times the pain levels of the placebo group.2,8,15,19 However, some authors15 found no significant difference between scores in this outcome after 4 weeks.
Kulekcioglu 200319 evaluated pain as an outcome by counting the number of pain points in the musculature, finding out that pain reduction in the LLLT group was higher.
Some authors2,6,9,13,19 evaluated jaw movements in terms of protrusion and laterality (in mm), finding out an increase in dimensions of these jaw movements after LLLT.
DISCUSSION
In recent years, the use of lasers in dentistry has become a popular noninvasive treatment2 with no side effects in terms of improvement of TMD symptoms, especially pain relief. As the treatment protocols available differ greatly from each other, professionals remain in doubt as to which the most effective is.
The pain produced by TMDs is intense and may interfere with a person’s daily activities. It also causes difficulty in terms of jaw movements, decreasing chewing ability and quality of nutrition,20,21 and consequently patient’s quality of life.
The clinical trials evaluated show that different types of laser have been proposed to reduce TMD symptoms. All show different effects on analgesia, some without significant differences from the placebo (Emshoff et al 20085 and Demirkol et al 201517). Others (Cetiner 20062 and Mazzetto 20106) have used the same type of laser, showing significant analgesia 3 and 4 times higher than those of their control groups. However, these differences reveal a variety of outcomes, which are not comparable with each other because the doses used were different, demonstrating the difficulties in making comparisons by meta-analysis to find evidence of one treatment being superior to another in order to establish a standardized protocol.
The laser type most commonly used for analgesia was GaAlAg.2,4,6,7,11-13 Although different doses were involved, this finding suggests that the GaAlAg laser should be the principal type to be tested in future standardized randomized clinical trials, measuring its outcomes to obtain evidence.
This systematic review shows that different wavelength types have been used and that most researchers report favorable results in terms of TMD symptom remission when using average lengths of 646 and 947 nm. It is known that the LLLT wavelength is related to the degree of penetration according to different clinical needs.22,23 It has been well established that infrared lasers with longer wavelengths have more penetrative power and have been the most used in clinical trials, with wavelengths of 830 nm, 904 nm and 1064 nm.13,17,19 However, some authors (Emshoff 20085 and Pereira 20148) have demonstrated the use of red lasers (632 nm and 660 nm) in the improvement of pain symptoms in their LLLT groups.
Regarding energy and density values, only two studies (Mazzetto et al6 and Venezian et al. 201015) used the same power of 50 mW. Others2,5,6,14,16 used different power settings ranging from 17 mW to 500 mW. Thus, concerning this parameter, the data were too variable to compare. However, it is known that establishing these values is very important since there is a high possibility of causing microthermal damage at the cellular level.23
In addition to wavelength and energy, another very important aspect of LLLT is the number of sessions and the laser application time required to cause biochemical reactions to produce the analgesic and anti-inflammatory effects, which must be exact for each case according to pain intensity. There is also no agreement among authors in this regard. What we can conclude is that an average of nine sessions2,6,7,13,15,17 with monitoring every 4 to 5 weeks appears to produce results favorable to the reduction of TMD symptoms.
Temporomandibular dysfunctions reduce quality of life due to the presence of pain, limitations in mouth opening and difficulty in performing lateral movements and protrusion of the jaw. Not all researchers choose to evaluate the same parameters.13 We found out that most researchers partially evaluate pain as a TMD parameter, possibly due to its wide range and intensity. Pain is a subjective sensation, and we found great variability of measurement methods and results in the clinical trials studied. This outcome may be questionable from the point of view of precision when interpreting whether the laser therapy worked or not. Mouth opening and range of jaw movements might be more objective parameters to determine whether a therapy had a beneficial effect.
Regarding the evaluation of pain by palpation of soft points, the group treated by laser reported pain reduction, compared with the group that received placebo. There is no consensus regarding how to evaluate muscle pain points, which makes it difficult to establish replicable and viable protocols. Some clinical trials measured each muscle in isolation,6 while others conducted the evaluation by identifying pain points around the TMJ region.19 This variability in evaluation techniques also leads to a lack of standardization.
The difficulty in mouth opening is an important component of symptomology; however, not all studies considered this outcome.5,14,16,17,19 Da Silva et al 201213 and Lima et al 201324 reported a significant improvement in mouth opening; however, other clinical trials also showed clinical improvement in the laser-treated group, but with lower statistical significance.11,13,24
The difficulty in chewing was not evaluated in most clinical trials. Only Cetiner et al 20062 evaluated this factor as an outcome. Some authors6,9,19 evaluated jaw movements in terms of protrusion and lateralization. These findings suggest that other clinical trials should be conducted to establish a protocol for treating TMD symptoms. Perhaps a clinical trial involving a larger number of objective parameters for diagnosis and comparing the outcomes of different therapies would be more powerful in terms of verifying the therapeutic effectiveness of laser treatment.
Finally, this systematic review shows that there are no established LLLT protocols for decreasing TMD symptoms, whether in terms of wavelength, power, energy density, or number of sessions. Nevertheless, each study has shown in its own way that the therapy under evaluation is effective in terms of symptom remission.