INTRODUCTION
The emergence and optimization of manufacturing processes using CAD/CAM (computer- aided design/computer-aided manufacturing) and rapid prototyping (3D printing) have enabled its implementation in various technical production areas. Dentistry, in its clinical and laboratory-related components, has not been oblivious to this phenomenon. It is increasingly common to see the use of desktop or intraoral scanners1, specialized design software2, Computerized Numerical Control (CNC) milling machines,3 and 3D laser stereolithography printers or DLP (Digital Light Processing)4 in workflows. The aim of introducing this technology is to replace the stages that characterize analogous workflows, such as taking impressions with elastomeric materials, plaster casting, polymer preparation, and analogous design and manufacturing of restorations or prostheses, among others. Such analogous workflows entail a high dedication of man-hours per job, in addition to the possibility (inherent to the human factor) of making errors in the preparations during the process. Typically, a 100%-digital workflow begins with taking the patient’s impression by means of an intraoral scanner. A digital model is thus obtained in STL (Standard Tessellation Language) format, which is used for designing the restoration using dental CAD software. Finally, the restoration’s design is sent to subtractive (CNC) or additive (stereolithography) manufacturing equipment for manufacturing5,6. These processes guarantee a significant reduction in clinical and laboratory work times, in addition to minimizing errors attributed to the human variable, theoretically obtaining greater reproducibility and precision in the preparations.
Despite the advantages mentioned above, new technologies have introduced other sources of error to the process, including scanners’ precision and resolution, designer skill, number of axes of the CNC milling machine, milling-cutter diameters, equipment calibration, shrinkage of printed parts, positioning of the part for manufacturing, and types of materials for milling and 3D printing. These can make the preparations likely to mismatches or discrepancies1,7,8, impairing the restoration’s performance and, therefore, reducing its lifetime. Out of all the factors mentioned above, the type of material for milling and 3D printing not only influences the restoration’s final fit on the preparation, but it also determines its mechanical properties, which, depending on its final application, can be decisive for adequate clinical performance.
Considering only polymeric materials, the most conventionally used one for provisional- restoration analog manufacturing is PMMA due to its biocompatibility, ease of handling and mechanical performance9. Additionally, this polymer’s mechanical, chemical and tribological properties make it an optimal material to be used in CAD/CAM technology as well, which allow for the manufacturing of crowns, bridges, and denture bases from dense PMMA blocks or discs. Moreover, stereolithography uses acrylic for printing temporary teeth10, denture bases11, clear retainers for invisible orthodontic treatments12, veneers13, etc. Depending on its final application, each resin must have different characteristics and properties that guarantee the ideal performance of the printed piece. In particular, printings made out of denture base resin must meet mechanical, chemical, and physical requirements, regulated by the ISO 20795-1 standard (Dentistry - Base polymers - Part 1: Denture base polymers), being flexural strength and elastic modulus highly important parameters.
Unlike PMMA-based acrylics, the mechanical properties of 3D-printing resins for denture bases have not been thoroughly analyzed. This is because they are commercially new products, and because there is no single formula: each specialized company commercializing this type of material produces its own formula, with a unique composition. Therefore, there is currently no certainty about the mechanical performance of these resins, apart from what the producer specifies in the technical datasheet.
The purpose of this comparative study is to evaluate the differences between the mechanical properties of conventional PMMA, monolayer PMMA blocks used for CAD/CAM processes, and 3D-printing acrylic resins used for denture bases. In order to achieve this, three null hypotheses were proposed:
-
There are no statistically significant differences between the flexural strengths of the evaluated polymers.
-
There are no statistically significant differences between the elastic moduli of the evaluated polymers.
-
There are no statistically significant differences between the compression strengths of the evaluated polymers.
METHODS
Preparation of test specimens
Conventional PMMA
For the manufacturing of the conventional PMMA (PC) test specimens, the Veracril heat- polymerized acrylic (New Stetic S.A.) was used. It was mixed in a 3:1 volumetric proportion with methyl methacrylate (MMA) monomer in a ceramic container. The mixture was left to stand for 10 minutes, which is the time necessary for surpassing the plastic stage according to the product’s use instructions. It was then deposited in mechanical pressing molds for the manufacturing of flexural strength (60x10x3mm) and compressive strength (4mm-diameter and 8mm-height) test specimens. The molds were pressed to 2000 psi during 5 minutes in a laboratory hydraulic press and later they were taken to a thermal reservoir, where a heating curve of 73°C was applied for 90 minutes, and then a curve of 95°C was applied for 30 minutes. Finally, the molds were removed from the reservoir and left outdoors for cooling.
CAD/CAM PMMA disk
A 98.5mm-diameter and 20mm-thick PMMA (CC) monolayer disk of the brand Portux (New Stetic S.A.) was used to manufacture test specimens for flexural (60x10x3mm) and compression strength (4mm diameter and 8mm height) in a Roland DWX-51D milling machine with the aid of the MillBoxLAV software, from STL models (Figure 1A).
3D resin
Mechanical-characterization test specimens were manufactured in a 405nm ASIGA PICO2 DLP printer from the STL files shown in figure 1A. In order to do that, a 3D-printing resin for denture bases, developed by New Stetic S.A (NS), and a NextDent Base (ND) resin, by NextDent B.V. were used. Both compression and flexural test specimens were printed vertically without supports (Figure 1B), using a layer thickness of 50μm. After the printing process, the parts were removed from the platform and cleaned in ethanol with the aid of an ultrasonic cleaner for 10 minutes. They were then post-cured for 15 minutes in a NextDent LC-3DPrintBox UV curing chamber.
Immediately after preparing the flexural-strength test specimens by applying any of the 3 methods, they were immersed in distilled water at 37°C for 50 hours, as specified by the ISO 20795-1:2013 standard14. Table 1 summarizes the evaluated materials.
Mechanical characterization
Flexural strength and elastic modulus
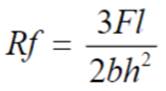
Flexural-strength tests were carried out according to the ISO 20795-1:2013 standard: After 50 hours of immersion in distilled water at 37°C, test specimens were brought to an INSTRON 4202 universal testing machine, where they were failed inside a water bath at 37°C, using a travel speed of 0.75mm/min. Five test specimens were failed for each manufacturing technique. Flexural strength was determined by using the following expression:
Where F is the maximum force exerted on the test specimen (N), l is the distance between the specimen supports (mm), b is the specimen width (mm), and h is the specimen thickness (mm).
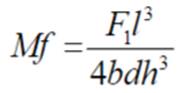
The following equation was used to calculate the elastic modulus:
Where F1 is the force exerted on the test specimen to a deflection of 2mm (N), l, b and h correspond to the distance of the supports, and the width and thickness of the test specimen, respectively (mm), and d is the deflection in millimeters to force F1, i.e., 2mm.
Compressive strength
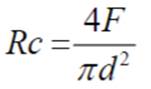
Compression-strength test specimens were immersed in distilled water for 24 hours at 37°C immediately after being manufactured. The compression strength test was performed in dry conditions, using a universal INSTRON 4202 testing machine, and a travel speed of 0.5mm/ min, at a temperature of 23°C. Compression strength was determined according to the following expression:
Where F is the maximum force applied to the test specimen (N), and d is the diameter of the test specimen (mm).
Statistical analysis
The collected data were analyzed descriptively with a one-way analysis of variance (ANOVA). Additionally, Tukey’s multiple test was used to determine significant differences between groups (α = 0.05). The analyses were performed by using the statistical package STATGRAPHICS Centurion XVI version 16.2.04.
RESULTS
Table 2 presents the average value of the evaluated resins’ flexural strength, elastic modulus, and compression strength, with their respective standard deviation. The average flexural strength values obtained were 78.35, 81.99, 83.51 and 87.48MPa for PC, CC, NS and ND polymers, respectively. The ANOVA analysis (Table 3) showed significant differences between the groups’ flexural strength values (P> = 0.01). Tukey’s test for multiple comparisons (Table 4) confirmed statistically significant differences between the conventional polymer (PC) and NextDent Base resin (P < 0.05). However, no differences were evident among the CC, NS and ND groups.
Table 2
Average values and standard deviation (SD) determined for flexural strength, elastic modulus, and compression strength of the evaluated materials. Additionally, the values reported in the respective technical data sheets (D.S.) are included
Table 3
One-way ANOVA analysis for the specific mechanical properties
Table 4
Comparison in pairs using the Tukey’s test. Asterisks (*) indicate statistically significant differences (Sig. diff.) between the evaluated pairs
Similarly, the average values of the elastic moduli obtained for the studied groups were 2224.41 (PC), 2125.43 (CC), 2208.76 (NS) and 2277.72MPa (ND). Neither the analysis of variance nor Tukey’s yielded significant differences between the evaluated groups.
Compression strength was higher than 80MPa in all cases, and 3D-printing resins (NS and ND) had values above 100MPa. Tukey’s test determined that there are significant differences between all evaluated groups, except between the conventional polymer and the CAD/CAM one.
DISCUSSION
In this work, the mechanical properties, and more precisely, the flexural strength, elastic modulus, and compression strength of 4 polymeric materials for denture-base manufacturing were determined. Based on analyses of variance, which demonstrated significant differences between the groups evaluated in terms of flexural and compression strength, null hypotheses were rejected for these mechanical properties, while the null hypothesis for the elastic modulus was accepted.
Dental prostheses must meet biocompatible, aesthetic, and mechanical requirements. The properties evaluated in this study are considered to be of great importance for the proper performance of dental prostheses, since they are subjected to flexural and compressive loads during bite actions and masticatory processes. Additionally, bending overload fracture is clinically considered to be the most common failure of denture bases15. Therefore, it should be ensured that prostheses do not have plastic deformations or fractures during their use in the mouth. Thus, high values of stiffness, flexural and compression strength16 are desired. Flexural strength, determined in a universal testing machine under wet conditions and at body temperature allows for the simulation of the material’s response to the mechanical loads to which it will be subjected during the masticatory process. At the same time, the elastic modulus indicates the stiffness or resistance offered by the material to being irreversibly deformed. Both properties are regulated by the ISO 20795-1 standard, which requires minimum values of 65MPa in flexural strength and 2000MPa in elastic modulus for heat-polymerized polymeric materials that are expected to be used for the manufacturing of denture bases. Consequently, from a mechanical point of view, all materials characterized in this study can be used as materials for such application. Nonetheless, ISO 20795-1 does not specify those values for photopolymerized polymers, such as 3D-printing resins, and thus far, there is no standard for regulating such materials. For this reason, the mechanical requests for heat-polymerized acrylics are assumed to assess the suitability of 3D resins for the above-mentioned application. On the other hand, compression strength is not a normative property according to ISO 20795-1, at least for this application, but it must be considered for this purpose, given that in areas such as the posterior teeth, the prosthesis is subjected to compressive efforts17.
The polymers analyzed in this work can be classified into two large groups according to their chemical nature: The first one includes PC and CC materials, both being heat-polymerized PMMA polymers. Specifically, CAD/CAM blocks or disks are manufactured with PMMA using compression, and are polymerized using a heating curve, i.e., similarly to the conventional works on acrylic. The other group consists of 3D-printing resins, NS and ND, which, as mentioned above, are photopolymerized liquid acrylics. On the one hand, PMMA resins are monofunctional, linear-chain compounds, resulting in lower flexural strength and elastic modulus18. This was not evidenced in the mechanical characterization. Apart from the PC and ND comparison, the difference between the properties of the evaluated materials was not significant. This is due to the fact that PC and CC materials are reinforced with a crosslinking agent in order to obtain branched and/or crosslinked chains, which restricts their movement and results in an increase in mechanical resistances19. On the other hand, 3D-printing resins for dental applications are composed of monomers and acrylic oligomers that can be mono-, bi-, and even trifunctional, such as bisphenol A-glycidil dimethacrylate or urethane dimethacrylate20. This favors obtaining a highly crosslinked and, therefore, stiffer, and more resistant polymer. Similarly, it can be seen in Table 2 that the experimental values correspond to those specified in the corresponding product’s technical datasheets21-23, which apparently validates the information provided by businesses. However, no technical information reported by manufacturers was found for the compression strength of the evaluated polymers. This is because this property is not regulated by ISO 20795-1. Similarly, there is no technical information available for New Stetic 3D resin, as this is a product currently undergoing the development phase, and it is not yet being sold by the company.
The mechanical properties of 3D-printed polymers do not depend solely on their composition and chemical structure. Variables like printing parameters and post-curing process affect the mechanical performance of the pieces manufactured through this technology20. Additionally, stereolithography is an additive manufacturing technique, which means that the printing of pieces is made through the continuous overlapping of layers with certain thickness. The test specimens for flexure and compression made with NS and ND resins were printed vertically (Figures 1B and 2A), which means that the direction of the uniaxial load in the flexion tests was parallel to the layers of the test specimens, whereas the direction of the compression load was perpendicular (Figure 2B). Alharbi et al.25 assessed the influence of the printing direction of cylindrical test specimens in the compression strength of a resin used for temporary teeth. It was observed that vertically printed test specimens (layers perpendicular to the direction of the load) had significantly higher compression strength than horizontally printed test specimens (layers parallel to the direction of the load). This occurs because the load applied parallel to the layers that compose the test specimen induces the separation or delamination of these more easily than when oriented in a perpendicular direction. This would suggest an increase in the flexural strength of test specimens made with NS and ND resins if printed in such a way that the layers are perpendicular to the direction of the uniaxial load during the test. However, this would mean increasing the area of contact between layers, which could increase the parts’ degree of porosity, residual stress, and dimensional distortions by shrinkage26, thus counteracting the possible increase in mechanical resistance.
Figure 2
A and B. Arrangement of printing layers and layer orientation with respect to the uniaxial direction of the load of mechanical flexure and compression tests

Source: by the authors
Although the mechanical results obtained in this study are promising for 3D-printing resins, it is necessary to carry out subsequent preclinical and clinical studies where the mechanical resistance of dental prostheses, printed in different orientations and positions, is evaluated for the application of more complex flexure, tensile and compressive loads. This would allow the results to be extrapolated in a more assured manner to the actual application of such products.
CONCLUSIONS
The elastic modulus, flexural and compression strength of 4 commercial polymeric materials were determined for the manufacture of denture bases by analog or digital techniques. The findings of this work have led us to conclude:
-
All evaluated materials had strengths and elastic moduli greater than the minimum required by ISO 207095-1. Therefore, if evaluated only from a mechanical point of view, the materials are appropriate to be used for the manufacturing of denture bases
-
3D-printing resins had higher compression strength values than PMMA acrylics, while there were no statistically significant differences between the evaluated materials either in the strength or in the elastic modulus
-
It is necessary to evaluate the influence of the orientation of the layers of the 3D-printed test specimens on the mechanical properties of the materials.