INTRODUCTION
Since late 2019 and early 2020 there have been reports speaking about the emergence of a virus in China, SARS-CoV-2, which causes a severe acute respiratory syndrome called COVID-19.1,2) Although COVID-19 primarily attacks the respiratory system, it also appears to cause adverse effects on several organs and systems, as it produces alterations in clotting,3 taste, smell, skin alterations and even intraoral injuries.4 COVID-19 spread and began to affect more countries, displaying high contagion, complication and mortality rates.5 On March 2020, the World Health Organization (WHO) declared the outbreak a pandemic and countries had to take extreme measures in order to try to control its spreading.5,6,7,8) This situation significantly affected health services9,10,11) and dentistry was not the exception.12,13,14
This pandemic has so far entailed more than 31 million cases and more than 960 thousand deaths worldwide, as stated in the data of the John Hopkins Coronavirus Resource Center on September 21, 2020.15) In Colombia, according to the Colombian National Institute of Health (Instituto Nacional de Salud, INS), on that same date, there were 765,076 confirmed cases and 24,208 deaths, with a case-fatality rate of 3.2%.16 Likewise, up to September 21, 2020, 90 cases of dental personnel testing positive for COVID-19 were reported.16) In Colombia, the first COVID-19 case was reported on March 6, 2020. The Ministry of Health issued several statements, regulations and guidelines aiming to control the spreading of the virus. On March 12, 2020, the government declared a public health state of emergency over COVID-19 and arrangements were made to address COVID-19, still without restrictions on the dental services provision. On March 25, a measure called “preventive mandatory isolation” was implemented nationwide and thereafter only emergency dental services were allowed to function.17) On May 14 the Ministry of Health and Social Protection issued the “biosafety guidelines for the provision of oral health care-related services during the SARS- CoV-2 (COVID-19) pandemic”. This guideline defined the standards and recommendations for biosafety processes and use of personal protective equipment (PPE) necessary during emergency care and priority oral health procedures.18
Since the global declaration of the pandemic, the Ministry of Health and Social Protection of the country has issued several guidelines, protocols and orientations such as the cleaning and disinfection guidelines in health services due to the appearance of the new coronavirus (SARS- CoV-2) in Colombia (March 16, 2020),19) the action plan for the provision of health services during the containment and mitigation phases of the SARS-CoV-2 pandemic (COVID-19) (March 30, 2020) and the technical consensus on the biosecurity conditions against SARS- CoV-2 and the prevention of COVID-19 disease in the Health Sector (May 2020),20) among others. As of May 5, the Ministry of Health allowed not only emergency care but also priority dental care with special biosafety measures issued in the following documents: biosafety guidelines for the provision of services related to oral health during SARS-COV-2 pandemic (COVID-19),18 and guidelines for the restoration of health services in the mitigation and control phases of the health emergency over COVID-19 in Colombia21) (June 2020). These circumstances have a strong impact on dental health workers (DHW) and has even forced many dentists in the country to close their practices, having critical effects on oral health services and on the profession’s economic conditions.14
For many years and due to the fact that dental procedures entail a close contact with patients, which could result in contact with saliva or blood contaminated with various pathogens, dentistry has constantly worked on improving biosafety measures.22) The risk of infection by microorganisms such as HIV, hepatitis B, tuberculosis, among others, are challenges that dentistry has successfully faced for decades.23,24) However, as a consequence of the COVID-19 pandemic emergence, governments, regulatory bodies and health workers, including dentists, have promoted implementing additional preventive and protective measures before, during and after dental care, in an effort to reduce the contagion risk, both for OHWs and their patients.12,25,26 Various countries have reported changes in dental practice, which have been implemented to guarantee the minimum risk of contagion and quality care in oral health services for users during the COVID-19 pandemic.27,28,29) The new care protocols include telephone triage, increase of personal protection equipment (PPE) use, both for dentists and auxiliary personnel, use of oral rinses for patients, staggering appointments, aerosol control and many more procedures, so as to control the spreading of the virus.13,30,31 OHWs are currently facing a real challenge and, as mentioned by Ternera-Pulido “it is necessary to guarantee, on the one hand, to provide services in biosafety, availability, and sufficiency conditions, and, on the other, to guarantee work in conditions of dignity and justice for all oral health professionals.”14
Given the devastating impact that COVID-19 pandemic has had on every sector, particularly the health one, it is very important that OHWs, professional associations and people in charge of health and public policies decisions have access to studies with reliable data and representative samples as a means of making choices and creating future plans based on quality scientific evidence. To our knowledge, to date, there are no studies that inquire about the impact of COVID-19 on dentistry in Colombia. Subsequently, the objective of this study was to evaluate practice modification, use of personal protective equipment, biosafety measures, self-reported contagion prevalence, and risk perception of dentists during COVID-19 pandemic in Colombia.
METHODS
We conducted a cross-sectional study using an anonymous survey about the impact of COVID-19 pandemic on dentistry, between June 19 and July 24, 2020, among dentists working in Colombia. The questionnaire, which was part of a global survey,32) was validated (face and content validity, and reproducibility) in a pilot test.
In Colombia, the exact number of dentists is currently unknown, but a projection of the number of dentists for 2019 found that there could be around 55,993 dentists.33) Nonetheless, the number of dentists registered at the Health Departments who worked in the national territory that same year was 31,872.34 The sample size was calculated according to the population of registered dentists for the year 2019 using OpenEpi software (Open Source Epidemiologic Statistics for Public Health, version 3.01, AG Dean, KM Sullivan, MM Soe, Atlanta, GA , USA) and the sample was drawn by convenience sampling. Having estimated a confidence level of 99.9%, a prevalence of 50% of dentists who had completely stopped their clinical activity, and a 3% precision during the pilot test, we determined that a minimum sample of 2,749 participants was necessary. The study included dentists who worked for the Colombian National Health System, as well as dentists working at private or public clinics. The questionnaire included four domains (D): D1: sociodemographic aspects (sex, age, region, geographic region, job performance, specialization), D2: profession-related aspects and impact on career plans, D3: protocols and biosafety compliance aspects, and D4: knowledge, risk of contagion and perception aspects.
Age was determined as a continuous variable; however, for statistical analysis it was re-categorized into 4 age groups: young adult (22 to 35 years), adult (36 to 45 years), mature adult (46 to 59 years) and older adult (≥ 60 years).
The survey was approved by the Ethics Committee of the Fundación Universitaria CIEO- UniCIEO (number 101, act 62). This study considered the set of principles regarding human research of the Declaration of Helsinki by the World Medical Association. All survey respondents answered a question about informed consent included on the first page of the questionnaire where dentists could refuse or approve their participation in the study. The survey was produced and distributed through Google Forms, making the necessary adjustments to prevent it from being filled out twice on the same device. It was distributed by scientific associations of dentists, dental schools, and dental products businesses such as COLGATE by way of email and social media.
One of the researchers analyzed the anonymous data and verified its consistency and quality. Statistical analyzes were performed using STATA 16 (StataCorp, College Station, Texas). A descriptive analysis of the qualitative variables with absolute and relative frequencies was carried out, and for the continuous variable (age), the median and range were calculated because it had a non-normal distribution.
RESULTS
Sociodemographic aspects
Test-retest reliability was high with a kappa coefficient of 0.91 to 0.96 (CI: 0.77, 0.96). Altogether, 5,375 surveys were completed, yet five surveys were discarded due to errors in the information record, leaving 5,370 viable surveys. Considering that in total there are 31,872 registered dentists working in Colombia, the corresponding response rate for the survey was 16.84%.
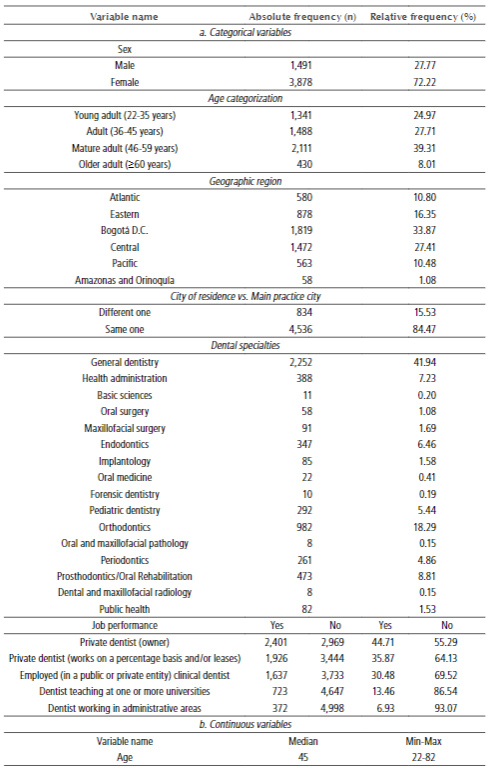
The study included dentists from all over the country. The average age was 45 years (22 to 82 years) and most of them were women (72.22%). The majority came from Bogotá DC (33.87%) and 27.41% came from the central region (Antioquia, Caldas, Quindío, Risaralda, Huila, Caquetá, and Tolima). Regarding their training, 41.94% were general dentists and 44.71% of those surveyed reported that they work in a private practice. 15.53% of the dentists reported that they work in a city other than their residence city (Table 1).
Profession-related aspects and impact on career plans
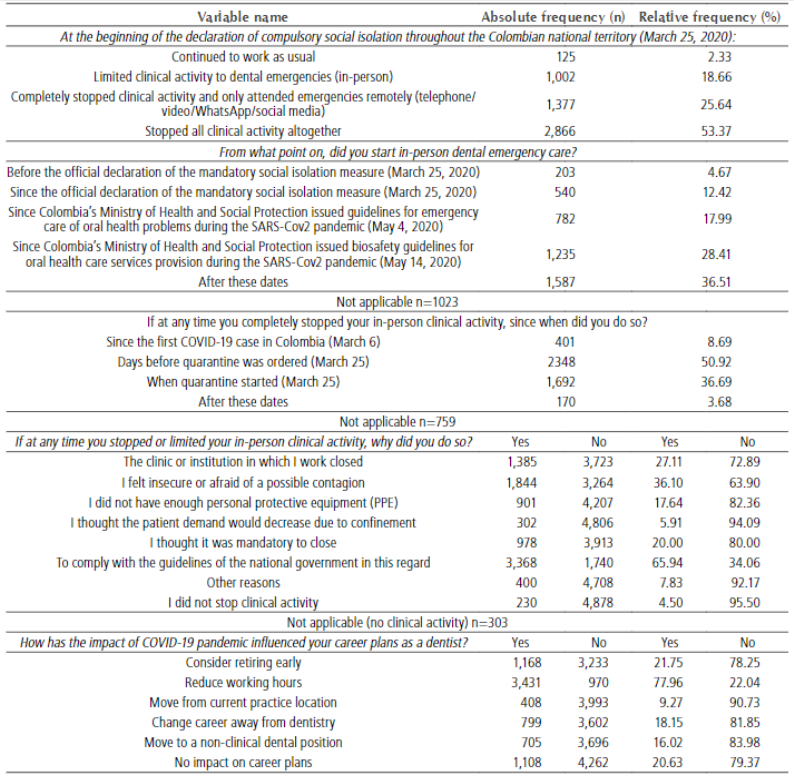
At the beginning of the mandatory social isolation measure, only 2.33% of dentists continued working as usual. On the subject of the resumption of in-person emergency care, since May 14, 63.49% of those surveyed already attended in-person emergencies and 36.51% did it after this date. The main cause to limit or stop in-person clinical activity was to comply with the guidelines of the national government (65.94%). In regard to the impact COVID-19 has had on career plans, 21.75% of survey respondents have thought about early retirement, while 77.96% have thought about reducing working hours (Table 2).
Protocol compliance and biosafety aspects
All (100%) survey respondents implement one or more protective measures such as preoperative mouthwash with 1% hydrogen peroxide (99.86%), surface disinfection (93.50%), hand washing (91.67%), patient health status assessment (90.16%), among others. Regarding the use of PPE, 89.65% used N95 or similar masks and 43.97% used surgical masks. In addition, 72.19% wore a reusable fluid-resistant gown and 100% wore a disposable fluid- resistant gown, sterile or not, as well as sterile (22.89%) or not sterile (91.45%) disposable gloves (Table 3).
Table 3
Biosafety measures at the dental practice and use of personal protective equipment (PPE) during the pandemic
Knowledge, contagion risk and perception aspects
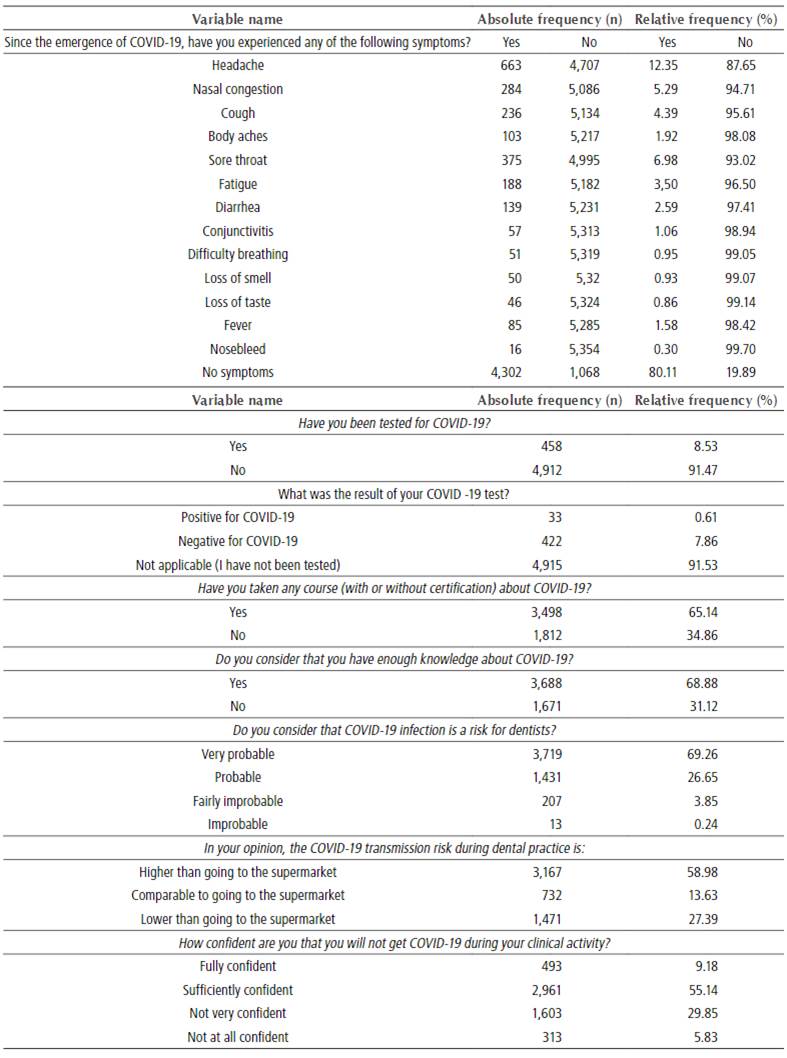
According to the reported data, 80% of dentists did not experience any COVID-19 related symptoms. Regarding the contagion risk perception, 69.26% considered that contagion is very likely in their clinical work (Table 4).
DISCUSSION
Sociodemographic aspects
This paper describes practice and career plans modifications, job performance, contagion risk, PPE use and biosafety measures that dentist in Colombia have implemented during the COVID-19 outbreak. Our sample consisted of a very high percentage of women (72.22%), which may be related to the higher proportion of female dentists in Colombia. In their report for Bogotá’s City Hall, Berdejo-Casas J and Ternera-Pulido J.34) asserted that out of all registered dentists in the country by March 2019, 75.46% were women. As for age, all age groups were represented in the sample. While the majority of the group was between 46 and 59 years old (39.31%), the percentage of older adults (³60) was the lowest (8.01%). A report made by the Special Registry of Health Service Providers (REPS) about the dentists registered on 2015 showed values similar to the ones observed in this study in relation to age groups.34 The most represented regions were Bogotá (33.87%) and Colombia’s central region (27.41%). This could be due to the national trend of having a higher concentration of dentists in urban areas with better internet and social media access or it could be due to the higher number of dentists in this urban areas that have good access to social media, through which the survey was distributed. The percentages that we found in our survey regarding the geographical distribution of dentists in Colombia are similar to the projections on this aspect of a report from the Ministry of Health for the Colombian Dental Federation (FOC) in September 2020.35 Therefore, the sample of this study could be considered a representative sample of dentists working in Colombia.
As far as dental specialties are concerned, we found that most respondents were general dentists (41.94%). This group is followed in number by orthodontists (18.29%), oral rehabilitation specialists (8.81%), health administration specialists (7.23%), endodontists (6.46%), pediatric dentists (5.44%) and periodontists (4.86%). According to the REPS in Colombia as to March 31, 2020, the larger number of records belonged to general dentists (20,651), followed by orthodontists (5,928), endodontists (2,744), periodontists (2,430), oral rehabilitation specialists (2,423) and pediatric dentists (1.546)14 Although the under- registration of oral health workers at the Ministry of Health must be noted, the results can still be comparable. It is plausible that the high number of responses from orthodontists may be due to the fact that two of the researchers are orthodontists and could have had more influence on their colleagues to answer the survey. Likewise, Colombian Society of Orthodontics provided great support by spreading the survey among its members.
In terms of job performance, only 44.4% of respondents are private dentists who own their practices or clinics and 35.87% work on a percentage basis or lease a place. The survey also revealed that 30.48% of dentists are employees, 13% are academics and 6.93% work in administrative areas. Ternera-Pulido J.33) found that among those offering oral health services in Colombia and registered at the Ministry of Health in 2018, 57% were independent professionals and 43% were public or private health care providers. Furthermore, 15.53% of survey respondents reported working in a city or town different to their place of residence. The previous results point towards the idea that this percentage of dentists have been deeply affected by the current pandemic in their capacity to provide oral health services seeing as in Colombia national flights were restricted until September and road trips between different departments also had restrictions during a similar period of time. Likewise, communities that mostly live in rural or remote areas where these dentists provided their services prior to the COVID-19 pandemic may have been deprived from oral health care, which can have a current and future impact on deepening the country’s inequity in oral health access.14
Profession-related aspects and impact on career plans
Since the national quarantine began in Colombia on March 25, 2020, due to the COVID-19 outbreak, oral health care services were suspended throughout the country and only emergency dental care was allowed. During that time, hardly any (18.66%) of the respondents attended emergencies, while 79.01% completely stopped in-person clinical activity. Only 35.08% attended emergencies before May 4 and 36.51% of respondents started providing clinical emergency care after May 14, 2020. Nearly 60% of respondents stopped in-person clinical consultation before the quarantine was enforced and 95.5% stopped or limited their clinical activity from March to May 2020, or even afterwards. This reported percentage is particularly high when compared to the percentages found by Tysi’c-Mi’ta M and Dziedzic A.13) in their study in Poland (71.2%), Ahmed and Jouhar et al.36) in a study including 650 dentists from various countries (66%) and Duruk G et al.37 (12.30%) in Turkey. The high rate of dental practitioners that stopped working found in our study might be explained by the specially restrictive Colombian government’s regulations regarding oral health care, the late issuance of biosafety guidelines for oral health emergency care and/or the professionals’ fear of becoming infected or infecting their families.36
As for the causes of stopping in-person clinical activity, 65% did so to comply with national government guidelines in this regard, 36% because they felt insecure, 17% because they did not have enough PPE elements, 27% because the clinic or institution where they worked closed and only 4.5% did not stop nor limit their clinical activity. In other countries, findings in this regard concur with our own. Tysiąc-Miśta M and Dziedzic A13) found that the main cause to halt clinical care was concern about their own or their families’ well-being (51.2% and 57.6, respectively), the second more common reason was lack of PPE (63.4%), as well as government regulations (53.5%). In their research, Duruk et al.37) and Ahmed MA et al.36 reported that more than 90% of the dentists surveyed were concerned about their safety and that of their families.
Employment status of dentistry in Colombia was already very complex before the COVID-19 pandemic on account of labor market flexibility, anti-competitive practices on clinic franchises’ rates, high costs and the psychological pressure that comes with government regulations establishing dental practices and discourages from attempting private consultation. For that reason, around 60% of dentists work for third parties, being subjected to poor working conditions, which in turn harm their material well-being and financial security14) Having said that, when facing unemployment and limitations to work due to government regulations, uncertainty and fear to contagion, working places closure and personal protective equipment (PPE) lack of availability and high costs caused by the COVID-19 outbreak, the employment status of private dentists that only earn money when seeing patients -being as they do not have a steady income- is devastating and will surely have effects on the community, if government and dental associations do not take action without delay. The unemployment rate for dentists in Colombia by 2020 was 30% without taking into account the COVID-19 pandemic.33) According to the National Administrative Department of Statistics (DANE) in July 2020 unemployment in Colombia reached 20.2% which meant an increase of 9.5 percentage points compared to the same month of the previous year (10.7%). This unemployment increase is attributable to the isolation measures aiming to contain the COVID-19 pandemic, which had a strong impact on the economy, including the dentistry labor market.38) Economic conditions of the dental profession not only affect dentists but also the human resources, industry and businesses that revolve around them, such as assistants, dental laboratory workers, enterprises, and dental units and products factories. Ternera-Pulido J.14) determined that by 2014, in Colombia the dental sector transactions per years amounted to a total of 2,138,220,000,000 COP (two trillion, one hundred and thirty-eight thousand and two hundred and twenty million pesos).
Based on this data, business administrator Mauricio Martínez Pinto carried out an economic projection for the FOC based on the 30.48% consumer price index (CPI), calculated with the projection of the values from 2014 into the five next years (2014-2019). He found that the indexed value for monthly expenditure generated by the dental industry at the end of 2019 averaged 232,495,124,621 COP (two hundred and thirty-two thousand four hundred and ninety-five million one hundred and twenty-four thousand six one hundred and twenty-one thousand pesos), which would annually represent 2,789,941,495,450 COP (two trillion seven hundred and eighty-nine thousand nine hundred and forty-one billion four hundred and ninety- five thousand four hundred and fifty pesos). Taking the above information as a reference, there is evidence to suggest that the losses caused by having stopped clinical activity in the dental sector for almost three months could be more than 700,000,000,000 COP (seven hundred trillion pesos). Bearing in mind that as this article is being written (September 2020) there are still plenty of restrictions, economical losses will surely be even bigger.
As for the impact of the COVID-19 pandemic on career plans as a dentist, 79.37% of respondents reported that it had some impact such as reducing their working hours (77.96%), considering retiring early (21.75%), switching to a career other than dentistry (18.15%), moving to a non-clinical position (16.02%) and changing the location of their practice (9.27%). Ternera-Pulido J.14) ascertained that according to the REPS, there was a decrease in registered oral health providers from March 2020 to July 2020, going from 38,216 registered providers to 37,450. Even if this decrease represents only 2% of qualified providers, some specialties such as oral surgery went from having 1,265 registered providers to 201, which constitutes a decrease close to 84%. Our research has highlighted the great impact of the pandemic, not only on current profession-related aspects but also on their future perspectives; consequently, if there are no strong public policies, easy access and low-interest loan plans, and a reduction in the burden and costs of licensing processes to motivate dentists to maintain their practices, it is likely that in the short term the dental sector crisis will be severe and, thus, Colombian people’s oral health will suffer the consequences. World Dental Federation (FDI) had envisioned as a goal of dentistry by 2020 “to substantially reduce inequalities in access to dental care and to meet the increasing need and demand for oral health care”.39) However, given the situation that dentistry is currently facing worldwide due to COVID-19 pandemic, these plans will be very difficult to fulfill, especially in developing countries that lack particular detailed plans to help OHWs, such as Colombia.
Protocol compliance and biosafety aspects
In the face of the COVID-19 pandemic contingency, several biosafety guidelines and manuals have been developed by the Colombian government entities, such as the Ministry of Health, as well as by the scientific community.18,19,20,40) All of them are consistent about the protective measures that health workers should take to reduce the contagion risk of SARS-Cov-2 virus. According to the document issued by the Ministry of Health and Social Protection in August 2020, which compiles all the guidelines and protocols to manage COVID-19 in Colombia, the suggestions for the basic PPE that health workers should use -depending on the generation of aerosols- are cap, face shield, N95 respirator, disposable gloves, fluid resistant uniform, fluid resistant gown, shoe covers or special footwear if performing aerosol-generating procedures. If the performed procedures do not generate aerosols, the suggestions remain the same, except for two elements: googles (instead of a face shield) and surgical mask (instead of a N95 respirator).20,41) In our research 90% of dentists reported using N95, FFP2 or FFP3 respirators, 56% surgical masks, and 13% elastomeric respirators. Cagetti et al.27) reported that 55% of respondents wore FPP2 or FPP3 respirators. Other studies36,37) have reported that only about 10% of dentists surveyed used N95 respirators in clinical care, which contrasts with our results indicating that 90% of dentists recount using it.
Regarding eye protection, of all our research participants, 96% responded that they wear a face shield and 79% wears protective glasses or googles. With regard to the clothing used, there was a high number of dentists who reported using both disposable (non-sterile, 35.85% and sterile, 67.75%) and reusable (72.19%) gowns, as well as a disposable caps (87.90%). They also reported using non-sterile (91.45%) and sterile (22.89%) disposable gloves and shoe covers (59.32%). These results suggest great observance in the use of PPE of dentists in Colombia. In some cases, they even use two elements for the same protective purpose, for example, protective glasses or goggles along with a face shield. This could be seen in the high percentages of responses for the use of these elements, since the respondent could choose one or several items at the same time.
On the other hand, rubber dams and rotating instrument with anti-retraction valve were not commonly used (22%). A possible reason for this could be that rubber sheets restrict areas to be treated in procedures that require all teeth to be visible, as in orthodontic treatments. As for rotating instrument with anti-retraction valve, their availability and prices could account for their limited use.
In our study, respondents reported great compliance with biosafety measures, having a response percentage higher than 85%. The implemented measures included surface disinfection, hand washing, taking body temperature, checking patient’s health status, making office adjustments, and using preoperative mouthwash, among others. These results could be explained by the prior existence of wide knowledge and compliance with most of these biosafety measures, as they already were part of the minimum qualification requirements deemed as mandatory by national Health Departments for dental practices qualification. Our findings significantly differ from what Duruk et al.37) reported in their study among Turkish dentists, who albeit taking certain precautionary measures against COVID-19, did not take enough to protect themselves, dental staff and patients. On the other hand, De Stefani et al.28 found that the lack of specific guidelines creates uncertainty on infection control and PPE use during dental practice in the current pandemic. Additionally, Singh Gambhir R. et al.29 found that around 86.2% and 94.2% of the surveyed dentists put hand washing and surface disinfection into practice in their clinical activities.
It is also important to consider the increase of consultation costs in order to guarantee PPE use and protective measures for oral health clinical care. A cost analysis conducted by the SCO’s cooperative (SCO life)42) estimated that the expenses for basic biosafety supplies per appointment for each patient were 12,277 COP. On top of that, we must add the current cost overruns on PPE caused by shortage, which increases their price up to ten times more than before the pandemic. It would be important for the National Government to recognize the great efforts of the OHWs in complying with the biosafety guidelines and using PPE, and to consequently create special price control plans for PPE and biosafety elements for dentists thorough the country.
Knowledge, contagion risk and risk perception on COVID-19 aspects
In the present study, 68.88% said they believe they have enough knowledge about COVID-19 and 65.14% reported having taken a course on the subject. Similar results have been found in other studies. In Italy, 84.4% of respondents reported that they had adequate knowledge about COVID-19,30 and in Turkey 69.8% of respondents reported having enough knowledge about COVID-19.37) Likewise, De Stefani et al.28) found that 70.2% of the respondents had accurate knowledge about COVID-19 symptoms; however, while 64.3% declared having been trained in infection prevention procedures, 48.7% reported not having COVID-19 specific knowledge to prevent its spreading. Kamate SK et al.31) found in a multinational study that 92.7% of those surveyed said they had good knowledge of the subject. In contrast to those findings, Singh Gambhir Ret al.29 found some notable deficiencies in the knowledge of COVID-19 fundamental aspects. Although more than 80% of survey respondents knew about COVID-19 transmission modes and symptoms, a third of the subjects did not knew about PPE use or COVID-19 treatment.
As regards of COVID-19 contagion among dentists, during the survey term (June 19 to July 24, 2020), 458 dentists reported having been tested for COVID-19, of which only 33 dentists reported testing positive, corresponding to 0.6% of the total sample. These data are in good agreement with the information from the INS, that reported on July 24 that there were 34 dentists infected with COVID-19.16 It should also be noted that as of September 21, 2020, this contagion report rose to 90 dentists with a positive COVID-19 test result in Colombia.
Another significant finding of our study is that of 5,370 surveyed dentists, 4,915 (91.53%) had not been tested for COVID-19, despite the fact that 20% reported having experienced some COVID-19 symptom. This suggests that despite dentists being considered at high risk, government authorities are not taking them into account in testing plans. It is essential for government policies to not only be restrictive on dentists work plans, but also develop complementary plans such as mass testing -which has proven to be an effective contagion prevention tool43- among the dental community, and support occupational risk companies and health services providers to allow them to provide effective and suitable services that ensure the security of OHWs, their patients and families.
The surveyed dentists also reported that for them COVID-19 infection is a risk (69.96%) greater than going to the supermarket (58.98%). Nevertheless, 64.32% said they are confident that they will not be infected with COVID-19 during clinical activity. This would appear to indicate that, although dentists in Colombia are aware of the risk of SARS-CoV-2 virus contagion, they are confident that they will not be infected in their consultations. These results might be explained by cultural features or by the confidence resulting from full compliance with biosafety measures and PPE use by dentists in Colombia. Matching results have been found in different countries by other authors in terms of COVID-10 contagion risk perception during oral health clinical activities, such as Putrino et al.30) in Italy where 87.5% of the respondents reported dental activities as a contagion risk situation, Duruk et al.37) found a 95% agreement in response to same question in Turkey and Ahmed MA et al36) found that 90% of respondents believe they can be infected. De Stefani et al.28 conclude that Italian dentists consider SARS-CoV-2 virus infection highly dangerous and are not confident in being able to carry out clinic activities safely.
During the COVID-19 pandemic, Colombian government has provided several benefits for health personnel such as physicians and nurses, for they are considered essential workers.44 However, it has not included DHWs within these plans, and so it is very important to regard Colombian people’s oral health as an essential service and the OHWs to be taken into account in employment protection plans, benefits and special loan plans that allow the economic resurgence of the entire dental sector in the country. The Ministry of Health has announced that once the vaccine against COVID-19 is available, the first priority group to be inoculated will be adults over 70 years of age, people with comorbidities (diabetes, hypertension, obesity, cancer, among others), and health workers.45 We -OHWs- hope that the government is considering us among the health workers who will receive these vaccines.
CONCLUSIONS
A total of 5,370 dentists working in Colombia were heard about the impact of COVID-19 on their clinical practice. We found a significant impact on every aspect that we studied, noticing modifications on clinical practice, PPE use, job performance, future plans and contagion risk perception. The percentages of reported use of PPE in clinical care and compliance with biosafety guidelines by dentists in Colombia are high, reaching almost 100%. Self-reported COVID-19 contagion among dentists was low (0.6%).
RECOMMENDATIONS
Further research should be undertaken concerning the pandemic’s impact on dentists personal, academic, professional, and work life. Besides, future studies should examine oral health status in different social groups within the framework of social isolation measures. Similarly, there is a need for policies and strategies in the workplace that allow to improve the dentist’s quality of life, since one of the profession challenges is to continue providing safe, quality, and profitable services, given that the pandemic has caused many additional costs related to the increase of needed PPE and other requirements for providing care to patients.