INTRODUCTION
Lipomas are benign neoplasms of adipose tissue. They are commonly encountered as sub- cutaneous tumors of the head and neck, shoulders, and back. Clinically, lipomas typically present as painless slow-growing, well-circumscribed yellowish masses, usually soft and mobile.1 Intraoral lipomas are infrequent, they represent less than 5% of all benign mesenchy- mal neoplasms of the oral cavity. They are predominantly found in the buccal mucosa, labial mucosa, and tongue; and their localization in the hard palate is infrequent. Histologically, the most common subtype is the conventional lipoma, followed by fibrolipoma, other variants such as spindle cell lipoma, angiolipoma, and chondrolipoma that represent less than 3%.2-4
The prevalence of fibrolipomas reported in recent case series of intraoral lipomas varies from 19.6 to 33%.2-4 Approximately, 251 cases of intraoral fibrolipomas have been reported, according to a PubMed search performed on case series and case reports, in English language, from 2000 to 2021 and using the keywords “oral fibrolipoma” (Table 1). They occur mainly in females in their seventh decade of life and present as a painless solitary nodule, normal- colored and with a slight prevalence for a sessile base.3,4 Buccal mucosa is the most affected site, followed by labial mucosa, tongue, alveolar sulcus, floor of the mouth, retromolar pad, ptherygomandibular raphe, and gingiva as the less common site. Palatal fibrolipomas are uncommon, they represent 7-14% of intraoral fibrolipomas.4,5 Microscopically, they are characterized by sheets of mature adipocytes admixed with dense bands of collagenous fibrous tissue.4 Their treatment is the surgical excision, and histopathological study is mandatory since it presents clinical similarity with other benign soft tissue reactive and neoplastic lesions. In general, clinical(differential?) diagnoses for intraoral fibrolipomas include mostly fibrous hyperplasia, lipoma/fibrolipoma, and other reactive conditions.4
This case report aims to present a pedunculated fibrolipoma of the hard palate, which is considered a very infrequent anatomical site and clinical feature of the oral cavity?
Table 1
Cases of fibrolipoma affecting the palate reported in the literatura
| rticle type | Author | Number of cases | Gender/ Age | Duration (months) | Clinical presentation | Clinical differential diagnosis |
|---|---|---|---|---|---|---|
| Case series | Said al Naief, 200111 | 4 | NS | NS | NS | NS |
| Case report | Fonseca, 200912 | 1 | M/35 | NS | Firm, rubbery, normal-colored sessile nodule | Pleomorphic adenoma, lymphoma, malignant neoplasm of salivary glands |
| Case series | Manjunatha, 201013 | 1 | M/70 | 6 | Painless, well-circumscribed, solitary, sessile, and normal-colored sub-mucosal nodule | Fibroma |
| Case series | Allon, 201110 | 4 | NS | NS | NS | NS |
| Case series | Naruse, 20155 | 1 | M/70 | 12 | Painless, normal-colored | NS |
| Case series | Linares, 20192 | 1 | NS | NS | Painless nodule | NS |
| Case report | Hayashi, 202014 | 1 | F/85 | 84 | Painless, smooth-surfaced, sessile, slightly yellowish mass | Lipoma |
| Case series | Pires, 20214 | 4 | NS | NS | NS | Fibrous hyperplasia, Lipoma/Fibrolipoma, other reactive conditions |
| Case report | Present case | 1 | F/70 | 240 | Painless, well-circumscribed, solitary, pedunculated, and normal-colored mass | Fibrous hyperplasia |
CASE REPORT
A 70-year-old female presented to the oral and maxillofacial surgeon complaining of mild pain on mastication. She mentioned that for 20 years she has had a swelling in her palate, which never caused pain. Intraoral examination revealed a well-circumscribed, pedunculated, elongated, and lobulated mass, arising from the anterior and lateral part of the palatal mucosa, particularly behind the upper left lateral incisor. The lesion was characterized by a pink and smooth non-ulcerated surface, measuring approximately 20 x 15 mm (Figure 1). During palpation, a fibroelastic consistency was detected. Her oral status was poor and multiple remaining roots were identified.
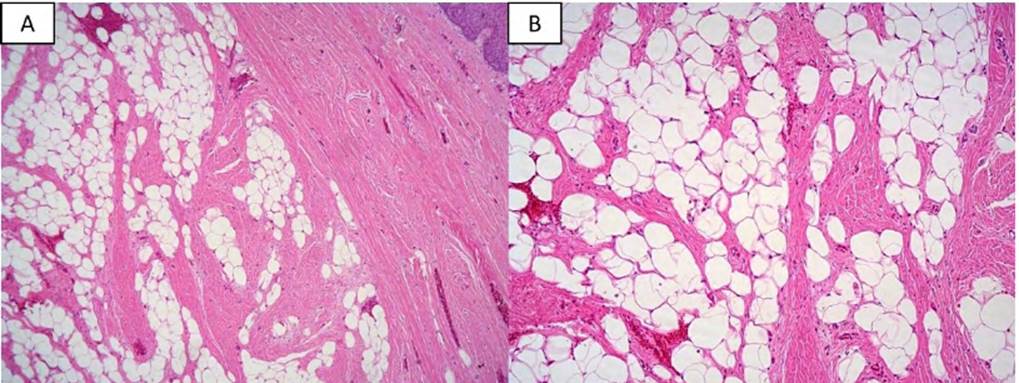
Based on the clinical features, fibrous hyperplasia was the main diagnostic hypothesis. However, the fact of being a long-standing lesion made it difficult to associate any source of trauma. Therefore, an excisional biopsy under local anesthesia was performed after obtaining the signed informed consent. The specimen was sent for histopathological analysis. Microscopically, it consisted of mature adipose tissue lobules, intersected by dense collagenous fibrous tissue bands covered by a squamous stratified parakeratinized epithelium. A fibrous capsule was seen surrounding the fibroadipose proliferation (Figure 2). The final diagnosis was fibrolipoma. The postoperative course was uneventful, and no recurrence was identified after 7 months of follow-up.
Figure 1
Clinical features: a normal-colored, elongated, and pedunculated swelling, with a smooth pink surface originating from the anterior and lateral hard palate mucosa

Source: by the authors
DISCUSSION
The hard palate is an infrequent site for adipose neoplasms as there is scarce adipose tissue in this area. In contrast, it is a common site for minor salivary gland neoplasms, harboring up to two-thirds of these cases. Most benign salivary gland tumors present with similar clinical features to other mesenchymal lesions, i.e. asymptomatic nodules with a smooth and normal- colored surface. However, and different from the present case, they are commonly sessile and found on the posterolateral aspect of the palate.6
Fibrous hyperplasia is the most common among the mesenchymal reactive lesions. It usually presents as a sessile nodule, and rarely exceeds 2 cm.7 Unlike this case, very often a source of chronic trauma is identified or related by the patients. Despite its high frequency, reactive hyperplastic lesions are uncommon in the palate, except for those associated with old or ill-fitting dentures.8
Regarding mesenchymal neoplasms, the palate is a frequent site for neural tumors. The most common in the oral cavity are neurofibroma and granular cell tumor, occurring in the palate and tongue, respectively. The hard palate is the most common intraoral site for palisaded encapsulated neuroma; however, it is usually a small submucosal nodule that rarely exceeds 1.0 cm.9
Classically, adipose lesions are associated with a yellowish discoloration; however, this color is only observed in 16.3% of intraoral lipomas. Most of them are covered by normal-colored mucosa as reported in the present case, and in these cases usually, lipoma is not considered a clinical differential diagnosis.3
Different from lipoma which has a male preponderance, fibrolipoma is more common in females, and regarding age, the latter is diagnosed in patients one decade older than simple lipoma, most of them in the seventh decade, as is our patient.10
Independent of histological variant, most of the intraoral lipomas are sessile based,4 particularly in fibrolipomas of the palate, when data were available, also most had a sessile base (Table 1). Interestingly, the actual case had a pedunculated base.
Due to their low frequency, there is few information about the clinical features and implications of the histological variants of intraoral lipoma. For this reason, it becomes important to properly diagnose and clinically characterize them as well as to differentiate them from other entities with similar characteristics.
CONCLUSION
Fibrolipoma is a benign lesion that mainly affects the buccal mucosa, and it is characterized as a painless, well-circumscribed sessile nodule with a normal-colored smooth surface. These clinical features are non-specific and could correspond to other entities, both reactive and neoplastic. The present case occurred in an unusual location for fibrolipoma, but common for salivary gland tumors, so histopathological examination is essential in order to achieve an accurate diagnosis.