INTRODUCTION
Third molars, with an average appearance of around 20 years of age1,2, usually face obstacles for an adequate eruption, representing 98% of the impactions, located mostly at the mandibular level3,4. There are also preponderant factors in the eruption pattern such as limited skeletal growth, distal eruption, verticalization in the growth of the condyle, the increase in the size of the dental crowns, and the delayed maturation of the third molars5. However, the eruption and possible impaction of these teeth is mostly linked to the space availability at the posterior ends of the dental arch6. Additionally, they can be linked to certain pathological conditions such as dental caries, periodontitis, pericoronaritis, external root resorption of the adjacent tooth, and the possible development of infections or cysts, among others7,8.
On the other hand, the extraction of third molars is considered one of the most frequent surgical procedures in oral surgery, even though it involves the possible occurrence of intra and post-operative complications9. One of them is the injury to the vascular-nerve bundle contained in the Inferior Alveolar Canal (IAC), caused by direct or indirect trauma10,11, with a prevalence of 0.4 to 8.4%12,13 that can have a significant impact on the quality of life of patients due to the damage caused to speech, chewing, etc14,15. However, these scenarios can be avoided with an accurate diagnostic imaging prior to the procedure, highlighting the importance of the panoramic radiography as a useful tool to evaluate the potential risk caused by the IAC, based on its proximity to the third molars due to the wide visualization it provides of the mandibular structures, condyles and possible nearby pathologies16. Despite the above, one of the disadvantages of the panoramic radiography is that it provides information only in two dimensions, so the absence of the cortical bone of the mandibular canal may not be evident with two-dimensional methods, and it would be complex to determine whether its direction is buccal or lingual to the roots. Consequently, it brings the attention to the presence of more accurate alternatives such as the Cone Beam Computed Tomography (CBCT), which is accepted for its high sensitivity in predicting exposure of the neurovascular bundle. CBCT is an effective method to locate the canal and its relationship with the roots of the lower third molars since it can generate images through the mandibular body in different planes. However, it should be mentioned that due to its high cost and limited availability, CBCT is not usually the radiographic technique of first choice for a pre-surgical evaluation of lower third molars in contrast to the panoramic radiography17. Additionally, thanks to digitalization, panoramic radiographs are an alternative that takes less time, reduces the radiation dose, and offers the possibility of improving the image by means of the computer18.
It is important to mention that there are several? classifications to evaluate the anatomical location of the third molars. The Pell and Gregory classification is based on the relationship between the level of this dental piece and the occlusal plane of the contiguous second molar. Therefore, it allows determining its relative depth as well as the relation it has with the ascending branch and the distal surface of the second molar19.On the other hand, the classification of Langlais et al. uses the IAC and its proximity to the roots of third molars as a reference point and it defines the presence of three types of images based on this relationship: dark band phenomenon, constriction of the diameter of the IAC, and discontinuity of the IAC20. However, due to the great variability observed in function to the IAC, it allowed the researchers of the academic section of Buccomaxillofacial Imaging of the Faculty of Stomatology at Universidad Peruana Cayetano Heredia, to postulate a modification of the mentioned classification, where besides appreciating the already known variants independently, two more signs were added: intact and change of direction of the IAC. It is important to mention that the latter is highly frequent in radiographic findings21.
The evidence refers to multiple investigations related to third molars and their complications; however, there are few studies about their location, especially in Latin America15,22. Therefore, the objective of this research was to determine the depth and proximity to IAC of third molars in panoramic radiographs of Latin American population.
METHODS
The present investigation was a cross-sectional study, with a sample, selected by convenience, and composed of a database of 6488 records of lower molars from digital panoramic radiographs, from patients between 18 and 65 years of age and of both sexes. This database belongs to the records of thesis research, carried out by 11 students of the second Professional Specialty international program in Oral and Maxillofacial Radiology of the Universidad Peruana Cayetano Heredia, from Bolivia (La Paz), Colombia (Bogotá and Nariño), Costa Rica (Guanacaste), Ecuador (Cuenca, Loja, Macas and Tungurahua), Mexico (State of Mexico) and Peru (Ayacucho and Lima), within the period 2010 to 2015.
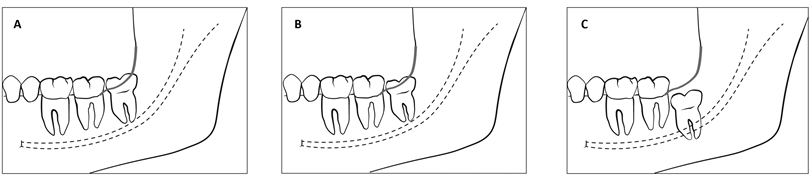
The students of the specialization program collected the information after an inter-examiner calibration process, having as a gold standard a professor specialized in oral and maxillofacial radiology with more than 20 years of experience, obtaining as a result a Kappa Index greater than 0.80 in all cases. The variables of the study were the depth of the lower third molar according to the classification of Pell and Gregory19 (figure 1), whose categories consisted of Position A when the highest point of the lower third molar is at or above the occlusal surface of the second molar, Position B when the highest point of the lower third molar is below the occlusal line but above the cervical line of the second molar, and Position C when the highest point of the lower third molar is at or below the cervical line of the second molar.
Figure 1
Aranda L.32 A. The highest point of the included tooth is at or above, the occlusal surface of the second molar. B. The highest point of the tooth is below the occlusal line, but above the cervical line of the second molar. C. The highest point of the tooth is, at or below, the cervical line of the second molar.
Fuente: por los autores
The proximity of the third molar to IAC was evaluated according to the proposed classification in this study that is based on a modification of Langlais et al’s classification20 (Figure 2). This establishes the following categories: Intact, when the roots of the third molar show no signs of proximity to the IAC; dark band phenomenon, when a radiolucent band is observed crossing the roots of the third molars; change of direction of the IAC, when it describes a marked curve close to the apical zone of the roots of the third molars; discontinuity of the IAC, when it is interrupted or non-existent when it crosses the roots of the third molars; constriction of the diameter of the IAC, when there is a decrease in its diameter that crosses the roots of the third molars; additionally, it is contemplated to include their different combinations. Furthermore, the variable was dichotomized into Intact and Proximal (in the latter, all other categories were grouped). Likewise, factors such as country, age, sex, and molar were considered as descriptive co-variables. With the database cleaned, the descriptive and bivariate analyses were performed; the tests used were Chi-square and Chi-square of linear trend for the associations of qualitative variables. For the mean differences, the Mann Whitney U and Kruskal Wallis tests were used, due to the absence of normality presented by the age variable, the Kolmogorov-Smirnov test was used. The analysis was developed in the STATA 17.0 program. Lastly, a confidence level of 95% and a p<0.05 was used.
Figure 2
Aranda L.32 A. Intact: The roots of the third molar do not show signs of proximity to the IAC. B. Dark band phenomenom: we observe a radiolucent band that crosses the roots of the third molars. C. Constriction of the diameter of the IAC. There is a decrease in the diameter of the IAC that crosses the roots of the third molar. D. IAC discontinuity: the IAC is interrupted or non-existent when it crosses the roots of the third molar. E. Change of direction of the IAC: the IAC describes a marked curve close to the apical zone to the roots of the third molars.

Fuente: por los autores
All the information collected, since it originated from research thesis, was approved by the Institutional Ethics Committee of the Universidad Peruana Cayetano Heredia with SIDISI registration No. 63901.
RESULTS
Regarding the proximity of the lower third molar to the IAC, according to the modified Langlais et al. classification, the highest frequency was Intact with 27.45% (n=1781), followed by Dark Band Phenomenon with 14.90% (n=967) and Dark Band Phenomenon + IAC Discontinuity with 12.87% (n=835). Regarding the depth of the third lower molar and according to Pell and Gregory, the most frequent were Position B with 46.90% (n=3043) and Position A with 46.75% (n=3033) and the least frequent was Position C with 6.35% (n=412). According to country, in the intact category, Peru had the highest frequency with 28.92% (n=515) and Costa Rica had the lowest frequency with 5.50% (n=124). Additionally, the variable country was associated with all variables (p<0.001) (Table 1). Likewise, the proximity and depth of the lower third molar were statistically different according to age (p<0.01) and sex (p<0.001) (Table 2). The overall proximity of the lower third molar to the IAC according to depth was 37.52% (n=1766) in Position A, in Position B it was 54.51% (n=2566) and Position C was 7.97% (n=375) and had an association between the variables (p<0.001) (Table 3).
Table 1
Frequency of the location of lower third molars according to countries in panoramic radiographs of Latin American population
Table 2
Frequency of location of lower third molars according to age, sex and molar in panoramic radiographs of Latin American population
| Location | n | % | Age | Sex | Molar | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| X | SD | p | Male | Female | p | Left | Right | p | |||||||
| n | % | n | % | n | % | n | % | ||||||||
| Proximity of the lower third molar to the IAC (Modified Langlais et al.20) | |||||||||||||||
| Intact | 1781 | 27.45 | 29.56 | 9.29 | <0.001** | 889 | 49.92 | 892 | 50.08 | <0.001*** | 909 | 51.04 | 872 | 48.96 | 0.177*** |
| Proximal | 4707 | 72.55 | 26.53 | 7.02 | 1878 | 39.90 | 2829 | 60.10 | 2314 | 49.16 | 2393 | 50.84 | |||
| Intact | 1781 | 27.45 | 29.56 | 9.29 | <0.001* | 889 | 49.92 | 892 | 50.08 | <0.001*** | 909 | 51.04 | 872 | 48.96 | 0.052*** |
| Dark band phenomenom | 967 | 14.90 | 27.58 | 7.46 | 366 | 37.85 | 601 | 62.15 | 491 | 50.78 | 476 | 49.22 | |||
| Change of IAC address | 35 | 0.54 | 26.51 | 5.27 | 17 | 48.57 | 18 | 51.43 | 20 | 57.14 | 15 | 42.86 | |||
| Discontinuity of IAC | 877 | 13.52 | 27.12 | 7.21 | 407 | 46.41 | 470 | 53.59 | 414 | 47.21 | 463 | 52.79 | |||
| Constriction of the IAC diameter | 237 | 3.65 | 26.59 | 6.62 | 91 | 38.40 | 146 | 61.60 | 111 | 46.84 | 126 | 53.16 | |||
| Dark band phenomenom + Change of IAC address | 89 | 1.37 | 27.24 | 7.76 | 26 | 29.21 | 63 | 70.79 | 47 | 52.81 | 42 | 47.19 | |||
| Dark band phenomenom + Discontinuity of IAC | 835 | 12.87 | 26.05 | 7.36 | 349 | 41.80 | 486 | 58.20 | 428 | 51.26 | 407 | 48.74 | |||
| Dark band phenomenom + Constriction of the IAC diameter | 147 | 2.27 | 26.25 | 6.52 | 66 | 44.90 | 81 | 55.10 | 70 | 47.62 | 77 | 52.38 | |||
| Change of IAC address + Discontinuity of IAC | 89 | 1.37 | 25.63 | 5.75 | 25 | 28.09 | 64 | 71.91 | 55 | 61.80 | 34 | 38.20 | |||
| Change of IAC address + Constriction of the IAC diameter | 99 | 1.53 | 25.29 | 5.72 | 36 | 36.36 | 63 | 63.64 | 44 | 44.44 | 55 | 55.56 | |||
| Discontinuity of IAC + Constriction of the IAC diameter | 302 | 4.65 | 25.83 | 6.16 | 134 | 44.37 | 168 | 55.63 | 143 | 47.35 | 159 | 52.65 | |||
| Dark band phenomenom + Change of IAC address + Discontinuity of IAC | 106 | 1.63 | 24.84 | 5.49 | 40 | 37.74 | 66 | 62.26 | 44 | 41.51 | 62 | 58.49 | |||
| Dark band phenomenom + Change of IAC address + Constriction of the IAC diameter | 48 | 0.74 | 27.94 | 7.36 | 8 | 16.67 | 40 | 83.33 | 19 | 39.58 | 29 | 60.42 | |||
| Dark band phenomenom + Discontinuity of IAC + Constriction of the IAC diameter | 535 | 8.25 | 25.36 | 6.56 | 202 | 37.76 | 333 | 62.24 | 278 | 51.96 | 257 | 48.04 | |||
| Change of IAC address + Discontinuity of IAC + Constriction of the IAC diameter | 117 | 1.80 | 26.91 | 6.59 | 38 | 32.48 | 79 | 67.52 | 48 | 41.03 | 69 | 58.97 | |||
| Dark band phenomenom + Change of IAC address + Discontinuity of IAC + Constriction of the IAC diameter | 224 | 3.45 | 26.34 | 6.79 | 73 | 32.59 | 151 | 67.41 | 102 | 45.54 | 122 | 54.46 | |||
| Depth of lower third molar (Pell and Gregory19) | |||||||||||||||
| Position A | 3033 | 46.75 | 28.59 | 8.67 | <0.001* | 1334 | 43.98 | 1699 | 56.02 | 0.008*** | 1538 | 50.71 | 1495 | 49.29 | 0.172*** |
| Position B | 3043 | 46.90 | 26.06 | 6.66 | 1240 | 40.75 | 1803 | 59.25 | 1494 | 49.10 | 1549 | 50.90 | |||
| Position C | 412 | 6.35 | 27.92 | 7.74 | 193 | 46.84 | 219 | 53.16 | 191 | 46.36 | 221 | 53.64 | |||
| Total | 6488 | 100.00 | 27.36 | 7.83 | 2767 | 42.65 | 3721 | 57.35 | 3265 | 50.32 | 3223 | 49.68 |
Table 3
Proximity of the location of the lower third molars according to depth in panoramic radiographs of the Latin American population
| Location | n | % | Depth of lower third molar (Pell and Gregory19 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Position A | Position B | Position C | p | ||||||
| n | % | n | % | n | % | ||||
| Proximity of the lower third molar to the IAC (modified Langlais et al.20) | |||||||||
| Intact | 1781 | 27.45 | 1267 | 71.14 | 477 | 26.78 | 37 | 2.08 | <0.001** |
| Proximal | 4707 | 72.55 | 1766 | 37.52 | 2566 | 54.51 | 375 | 7.97 | |
| Intact | 1781 | 27.45 | 1267 | 71.14 | 477 | 26.78 | 37 | 2.08 | <0.001* |
| Dark band phenomenom | 967 | 14.90 | 427 | 44.16 | 469 | 48.50 | 71 | 7.34 | |
| Change of IAC address | 35 | 0.54 | 7 | 20.00 | 24 | 68.57 | 4 | 11.43 | |
| Discontinuity of IAC | 877 | 13.52 | 395 | 45.04 | 450 | 51.31 | 32 | 3.65 | |
| Constriction of the IAC diameter | 237 | 3.65 | 98 | 41.35 | 120 | 50.63 | 19 | 8.02 | |
| Dark band phenomenom + Change of IAC address | 89 | 1.37 | 15 | 16.85 | 58 | 65.17 | 16 | 17.98 | |
| Dark band phenomenom + Discontinuity of IAC | 835 | 12.87 | 344 | 41.20 | 435 | 52.10 | 56 | 6.71 | |
| Dark band phenomenom + Constriction of the IAC diameter | 147 | 2.27 | 46 | 31.29 | 88 | 59.86 | 13 | 8.84 | |
| Change of IAC address + Discontinuity of IAC | 89 | 1.37 | 30 | 33.71 | 53 | 59.55 | 6 | 6.74 | |
| Change of IAC address + Constriction of the IAC diameter | 99 | 1.53 | 36 | 36.36 | 46 | 46.46 | 17 | 17.17 | |
| Discontinuity of IAC + Constriction of the IAC diameter | 302 | 4.65 | 105 | 34.77 | 156 | 51.66 | 41 | 13.58 | |
| Dark band phenomenom + Change of IAC address + Discontinuity of IADC | 106 | 1.63 | 26 | 24.53 | 69 | 65.09 | 11 | 10.38 | |
| Dark band phenomenom + Change of IAC address + Constriction of the IAC diameter | 48 | 0.74 | 8 | 16.67 | 28 | 58.33 | 12 | 25.00 | |
| Dark band phenomenom + Discontinuity of IAC + Constriction of the IAC diameter | 535 | 8.25 | 165 | 30.84 | 347 | 64.86 | 23 | 4.30 | |
| Change of IAC address + Discontinuity of IAC + Constriction of the IAC diameter | 117 | 1.80 | 26 | 22.22 | 68 | 58.12 | 23 | 19.66 | |
| Dark band phenomenom + Change of IAC address + Discontinuity of IAC + Constriction of the IAC diameter | 224 | 3.45 | 38 | 16.96 | 155 | 69.20 | 31 | 13.84 | |
| Total | 6488 | 100.00 | 3033 | 46.75 | 3043 | 46.90 | 412 | 6.35 |
DISCUSSION
Exodontia of mandibular third molars is a routine procedure in dental practice that, in case of complications, could lead to multiple scenarios. One of them is the injury to the lower dental nerve. In this sense, it is necessary to use diagnostic imaging methods such as the panoramic radiography, which provides with greater precision, a complete view of the number, location, and proximity of the roots to other adjacent structures that may be compromised such as the IAC16,23. However, due to its limitation of only providing two-dimensional information, CBCT is still the most accurate imaging alternative17.
As part of the findings of this investigation, in terms of the proximity of the mandibular third molars, we found that more than three-quarters of the third molars were found close to the IAC. These results coincide with those previously published by Huang et al., who determined that more than 80% of the mandibular third molars contacted or were superimposed on the IAC by using panoramic radiographs of 120 patients from a hospital in Taiwan24. However, there is limited scientific evidence using a standardized classification to identify the proximity of lower third molars to the IAC such as that presented by Langlais et al. and its modification, which is proposed in this paper.
On the other hand, according to Pell and Gregory's classification, the most frequent depth levels in this sample were A and B, together representing almost all the data. Regarding the type A depth level, Jaron et al. evaluated the depth of impaction of third molars with an indication for surgical extraction in the panoramic radiographs of 1585 patients from countries located east of the Baltic Sea, reporting that more than half of the cases showed this Depth25. This result is essential for our research because it coincides with the present study findings. Contrary to our study, an analysis carried out on Turkish people showed that, in the lower jaw, the C classification was the most common according to impaction depth. These findings differ from our study's; this could be related to certain factors like the objective population ethnicity, which is relevant when considering the type of treatment for the patients. Additionally, the auxiliary examinations for the Turkish study belonged to individuals with the indication for exodontia and acute symptomatology such as pain, pericoronaritis, lymphadenopathy, and trismus26.
However, due to the lack of evidence, it has not been possible to identify articles that associate proximity and depth using the same classifications used in this study. Regarding depth, Deshpande et al. demonstrated that digital orthopantomographies are a reliable tool to evaluate depth in third molars impacted with IAC. In addition, they observed that impactions with closer distances to the IAC presented radiographic signs indicating risk and compromising that structure; radiographic findings associated with the proximity between the tooth and the IAC, known as "interruption of the white line," are mentioned27. Similarly, the radiographic analysis allows classifying and determining that those mandibular third molars that maintain close contact with the IAC are linked to a high risk of nerve tissue injury as postoperative sequelae due to their proximity28.
It is important to mention that in this study the proximity to IAC and depth of the lower third molar presented significant differences in their distribution according to age and sex. Similarly, some authors previously state that women present third molars closer and more superimposed to the IAC in comparison to men. In addition, they express specific factors such as age and sex and they present a greater risk of injury to the IAC, according to the location of the structures involved29,30.
Among the limitations observed in this study, we highlight its cross-sectional design, which only allows us to describe the behavior of the variables, but not to infer causal relationships between them. Likewise, the lack of randomization to select the sample, in addition to the presence of non- homogeneous values for each country that allowed us to expose that these findings lack the power to be extrapolated, being only applicable to the sample of this research. In contrast, thanks to technological advances, the use of CBCT is recommended because the location of the mandibular lower third molar can be determined with greater precision.
In this regard, it is important to highlight the contribution that this research makes to the correct pre- surgical diagnosis, due to the high frequency of lower third molars that have close contact with the IAC, which could lead to postoperative complications that, if not considered, are detrimental to the patient. Although panoramic radiographs are widely used in specific contexts, such as countries under evaluation, it is essential to mention that when there is a proximity finding, it would be advisable to complement the diagnosis with a CBCT scan for greater certainty in the localization31. In addition, the findings of this study can be taken as the basis for the generation of further research using panoramic radiographs and the same parameters stablished in this study, including the modified Langlais et al. and Pell and Gregory classifications. Moreover, this is the first published research that modifies the Langlais classification to propose its own classification based on the theory applied to radiographic evidence.
CONCLUSION
According to the modified classification of Langlais et al, the majority of lower third molars in the Latin American population are close to the inferior alveolar canal; and according to the depth classification of Pell and Gregory, the most frequent depths are Positions A and B. In addition, proximity to IAC and depth were associated with each other and with the co-variables country, age, and sex.