Vibrio cholerae no o1/ no 0139 neuroinfection secondary to ventriculoperitoneal shunt: case report
DOI:
https://doi.org/10.17533/udea.iatreia.24Keywords:
cerebrospinal fluid, infection, ventriculoperitoneal shunt, vibrio choleraeAbstract
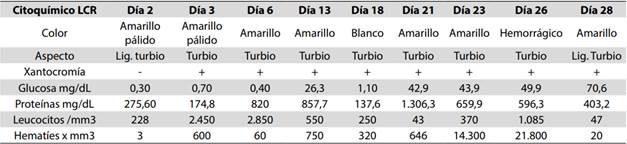
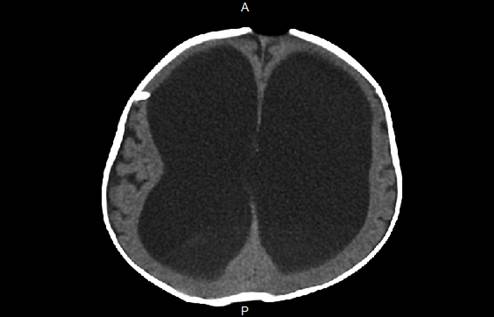
The infection of the ventriculoperitoneal shunt is one of most frequent complications for this procedure. Vibrio choleraO1 and O139 is a Gram negative bacteria known mainly for being responsible of the epidemic cholera, however, there are serotypes no O1/ no O139 capable of causing extraintestinal conditions, among them neuroinfection cases have been reported. We present the case of a 9 months old patient who after the placement of a ventriculoperitoneal shunt as treatment for connate obstructive hydrocephalus, presents a neuroinfection condition and valve malfunction syndrome, being able to isolate the Vibrio cholerae no O1/ no O139 in the cerebrospinal fluid and the tip of the catheter. It is the first report in the literature in which the Vibrio cholerae no O1/ no O139 is isolated in the cerebrospinal liquid secondary to an infection from a ventriculoperitoneal shunt.
Downloads
References
(1.) Ram Y, Tina QT. Infections Related to Prosthetic or Artificial
Devices. En: Cherry J. Demmler-Harrison G, Kaplan S, et al. Feigin and Cherry’s Textbook of Pediatric Infectious Diseases. 7th ed. Elsevier. 2014; 1029-30.
(2.) Jimenez-Mejias M, Garcia-Cabrera E. Infecciones relacionadas con los sistemas de drenaje de líquido cefalorraquídeo. Enferm Infect Microbiol Clin 2008;26(4):240-51. DOI 10.1016/S0213-005X(08)72696-X.
(3.) Gutierrez-Murgas Y, Snowden J. Ventricular shunt infections: Immunopathogenesis and clinical management. J Neuroimmunol. 2014;276(1-2):1-8. DOI 10.1016/j.jneuroim.2014.08.006.
(4.) Clemens J, Balakrish-Nair G, Ahmed T, Qadri F, Holmgren J. Cholera. Lancet. 2017; 390(10101):39-49. DOI 10.1016/S0140-6736(17)30559-7.
(5.) Anderson A, Varkey J, Petti C, Liddle R, Frothingham R, Woods C. Non-O1 Vibrio cholerae septicemia: case report, discussion of literature and relevance to bioterrorism. Diagn Microbiol Infect Dis. 2004;49(4):295-7. DOI 10.1016/j.diagmicrobio.2004.04.016.
(6.) West B, Silberman R, Otterson W. Acalculous cholecystitis and septicemia caused by non-O1 Vibrio cholerae: first reported case and review of biliary infections with Vibrio cholerae. Diagn Microbiol Infect Dis. 1998,30(3):187-91.
(7.) Ismail E, Shafik M, Al-Mutairi G. A case of non-O:1 Vibrio cholerae septicemia with meningitis, cerebral abscess and unilateral hydrocephalus in a preterm baby. Eur J Clin Microbiol Infect Dis. 2001;20(8):598–600.
(8.) Kerketta J, Chandran-Paul A, Balaji V, Kirubakaran C, Jesudason M, Moses P. Non-O1 Vibrio cholerae septicemia and meningitis in a neonate. Indian J Pediatr 2002, 69(10):909-0.
(9.) Villarejo F, Martínez J. Neurocirugía Pediátrica. Ergon; 2001.
(10.) Kanev P, Sheehan J. Reflections on shunt infection. Pediatr Neurosurg. 2003;39(6):285-90. DOI 10.1159/000075255.
(11.) Romero-Garcia M, León-Ramirez A, Carreón-Guerrero J, Romero-Garcia F. Factores de riesgo de infección del sistema de derivación ventriculoperitoneal en pacientes pediátrico. Enf Inf Microbiol. 2014;34(2):59-6.
(12.) Petsaris O, Nousbaum JB, Quilici ML, Le Coadou G, Payan C, Abalain ML. Non-O1, non-O139 Vibrio cholerae bacteraemia in a cirrhotic patient. J Med Microbiol. 2010; 59(Pt10):1260-2. DOI 10.1099/jmm.0.021014-0.
(13.) Lai CC, Liu WL, Chiu YH, Gau SJ, Hsueh PR. Spontaneous bacterial empyema due to non-O1, non-O139 Vibrio cholerae in a cirrhotic patient with hepatocellular carcinoma. Diagn Microbiol Infect Dis. 2012;73(1):84-5. DOI 10.1016/j.diagmicrobio.2012.01.011.
(14.) Farfan M, Miñana D, Fusté MC, Lorén JG. Genetic relationships between clinical and environmental Vibrio cholerae isolates based on multilocus enzyme electrophoresis. Microbiology. 2000;146(Pt10):2613-26. DOI 10.1099/00221287-146-10-2613.
(15.) Cabrera Rodríguez LE, Bravo Fariñas L, Ramírez Álvarez M, Llop Hernández A, Fernández Abreu A, Morier Díaz L, et al. Susceptibilidad a los antimicrobianos y factores de virulencia en cepas de V. cholerae no-O1 aisladas de pacientes con enfermedad diarreica aguda. Rev Biomed. 2008;19(3):138–44.
(16.) Fernandez-Abreu A, Bravo-Fariñas L, Rivero-Navea G, Cabrera-Cantelar N, Nuñez-Fernandez S, Cruz-Infante Y, et al. Determinants of Virulence and Antimicrobial Susceptibility in Non-O1, Non-O139 Vibrio cholerae Isolates. MEDICC Review. 2017; 19(4):21-5.
(17.) Leibovici-Weissman Y, Neuberger A, Bitterman R, Sinclair D, Salam MA, Paul M. Antimicrobial drugs for treating cholera. Cochrane Database Syst Rev. 2014;6:CD008625. DOI 10.1002/14651858.CD008625.pub2.
(18.) Deshayes S, Daurel C, Cattoir V, Parienti J-J, Quilici M-L, de la Blanchardiere A. Non-O1, non-O139 Vibrio cholerae bacteraemia: case report and literatura review. SprigerPlus. 2015;4:575. DOI 10.1186/s40064-015-1346-3.
(19.) Ghosh A, Ramamurthy T. Antimicrobials & cholera: are we stranded? Indian J Med Res. 2011;133(2):225-31.
(20.) Stypulkowska H, Pancer K, Roszkowiak A. Two unrelated cases of septicemia due to Vibrio cholerae non-O1, non-O139 in Poland, July and August 2006. Euro Surveill. 2006;11(11):E061130.2.
(21.) Igbinosa E, Okoh A. Emerging Vibrio species: an unending threat
o public health in developing countries. Res Microbiol. 2008;159(7-8):495-506. DOI 10.1016/j.resmic.2008.07.001.
(22.) Couzigou C, Lacombe K, Girard P, Vittecoq D, Meynard J. Non-O:1 and non-O:139 Vibrio cholerae septicemia and pyomyositis in an immunodeficient traveler returning from Tunisia. Travel Med Infect Dis. 2007;5:44-6.
(23.) Ayoub M, Laurence F, Arnaud C, Marret S, Vieux R, Aujard Y, et al. Neonatal Infection and 5-year Neurodevelopmental Outcome of Very Preterm Infants. Pediatrics. 2013;132(2):e372-e80. DOI 10.1542/peds.2012-3979.
(24.) Ros-López B, Jaramillo-Dallimonti A, De Miguel-Pueyo L, Rodríguez-Barceló S, Domínguez-Páez M, Ibáñez-Botella G, et al. Hemorragia intraventricular del prematuro e hidrocefalia post-hemorrágica. Propuesta de un protocolo de manejo basado en la derivación ventrículo-peritoneal precoz. Neurocirugía. 2009;20:15-24.
(25.) Brook I. Meningitis and shunt infection caused by anaerobic bacteria in children. Pediatr Neurol. 2002,26(2):99-105.
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.