Recommendations for visual exam in children
DOI:
https://doi.org/10.17533/udea.%20iatreia.v32n1a05Keywords:
amblyopia, visual acuity, children, vision screeningAbstract
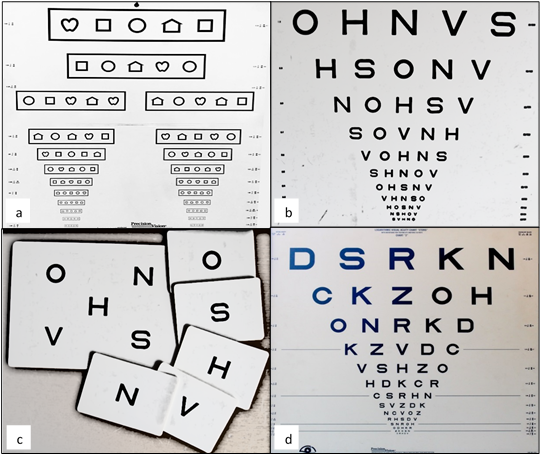
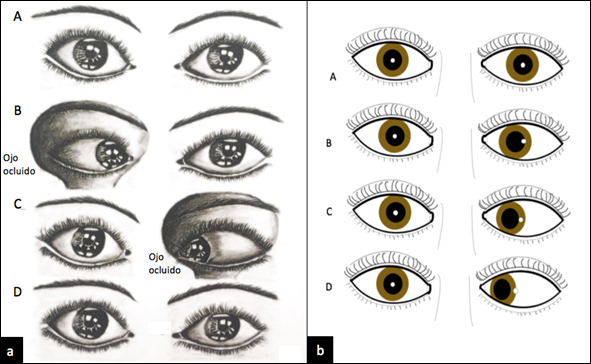
Introduction: Visual screening in children is an assessment that should be performed by the primary care physician to detect diminished visual acuity or risk factors that may interfere with an appropriate development of the eye and visual system. In the visual screening, visual acuity, ocular alignment and the presence of structural ocular anomalies should be assessed.
Methods: A literature review about strategies to perform an adequate pediatric visual examination by general physicians and pediatricians for early detection of visual problems in children was carried out.
Results: Visual disorders are one of the main causes of disability in children, being the main risk factors uncorrected refractive errors, strabismus and congenital cataracts, that can leave irreversible sequels if they are not detected on time, being those disorders identified through visual screening.
Conclusions: Whenever the visual acuity is detected below the expected for the patient’s age, poor fixation and/or follow after 3 months, muscle imbalance, alteration of the red reflex, etc., the child should be referred to a visual health professional to prevent permanent visual loss.
Downloads
References
(1.) American Academy of Ophthalmology. Pediatric Eye: Preferred Practice Pattern guidelines [Internet]. San Francisco: Elsevier; 2017. Available from: file:///C:/Users/Informatica/Downloads/Pediatric%20Eye%20Evaluations-FINAL-12.19.17.pdf
(2.) Tingley DH. Vision screening essentials: Screening today for eye disorders in the pediatric patient. Pediatr Rev. 2007;28:54-61. DOI 10.1542/pir.28-2-54.
(3.) Powell C, Hatt SR. Vision screening for amblyopia in childhood. Cochrane Database Syst Rev. 2009 Jul;(3):CD005020. DOI 10.1002/14651858.CD005020.pub3.
(4.) Parra AJ. Tamización de ambliopía en cuidado primario. Univ Med. 2009;50(2):225-36.
(5.) Donahue SP, Arnold RW, Ruben JB; AAPOS Vision Screening Committee. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003 Oct;7(5):314-6. DOI 10.1016/S1091-8531(03)00182-4.
(6.) Tailor V, Balduzzi S, Hull S, Rahi J, Schmucker G, Virgili G, Dahlmann-Noor A. Tests for detecting strabismus in children age 1 to 6 years in the community. Cochrane Database Syst Rev. 2014;(7):CD011221. DOI 10.1002/14651858.CD011221.
(7.) Chou R, Dana T, Bougatsos C. Screening for Visual Impairment in Children Ages 1-5 Years: Systematic Review to Update the 2004 U.S. Preventive Services Task Force Recommendation [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2011 Feb. Available from http://www.ncbi.nlm.nih.gov/books/NBK52708/
(8.) Williams C, Northstone K, Harrad RA, Sparrow JM, Harvey I; ALSPAC Study Team. Amblyopia treatment outcomes after screening before or at age 3 years: follow up from randomised trial. BMJ. 2002 Jun;324(7353):1549.
(9.) Tarczy-Hornoch K, Varma R, Cotter SA, McKean-Cowdin R, Lin JH, Borchert MS, et al. Risk factors for decreased visual acuity in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011 Nov;118(11):2262-73. DOI 10.1016/j.ophtha.2011.06.033.
(10.) American Academy of Ophthalmology. Pediatric ophthalmology and clinical strabismus. BCSC: San Francisco, CA; 2016- 2017.
(11.) Reiff A, Kadayifcilar S, Özen S. Rheumatic inflammatory eye diseases of childhood. Rheum Dis Clin North Am. 2013 Nov;39(4):801-32. DOI 10.1016/j.rdc.2013.05.005.
(12.) Heiligenhaus A, Heinz C, Walscheid K, Foeldvari I. Uveitis in Children. In: Zierhut M, Pavesio C, Ohno S, Orefice F, Rao N. Intraocular inflammation. Berlin: Springer; 2016. p. 618-18. DOI 10.1007/978-3-540-75387-2_48.
(13.) Clarke L, Guex-Crosier Y, Hofer M. Epidemiology of uveitis in children over a 10 years period. Pediatric Rheumatology. 2011;9(Suppl 1):223. DOI 10.1186/1546-0096-9-S1-P223.
(14.) Organización Panamericana de la Salud, Organización Mundial de la Salud. Guía de práctica clínica para el manejo de la retinopatía de la prematuridad [Internet]. Washington, D.C.: Pan American Health Organization; 2017 [citado Abril 2018]. Disponible en: http://iris.paho.org/xmlui/handle/123456789/34948
(15.) Zuluaga C, Sierra MV, Asprilla E. Causas de ceguera infantil en Cali, Colombia. Colomb Med. 2005;36(4):235-38.
(16.) Birch E, Castañeda Y, Wheaton D, Birch D, Uauy R, Hoffman D, et al. Visual maturation of term infants fed long-chain polyunsaturated fatty acid-supplemented or control formula for 12 mo. Am J Clin Nutr. 2005;81:871-9.
(17.) Organización Mundial de la Salud. Ceguera y discapacidad visual [Internet]. Ginebra: WHO; 2014 [cited 2014 Aug]. Available from: http://www.who.int/mediacentre/factsheets/fs282/es/
(18.) World Health Organization. Universal eye health: a global action plan 2014-2019 [Internet]. Ginebra: WHO; 2017 [cited 2017]. Available from: http://www.who.int/blindness/actionplan/en/
(19.) Colombia. Ministerio de Salud. Análisis de situación de salud visual en Colombia 2016 [Internet]. Bogotá: MinSalud; 2016 [citado 2016]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ENT/asis-salud-visual-colombia-2016.pdf
(20.) Doshi NR, Rodriguez ML. Amblyopia. Am Fam Physician. 2007 Feb;75(3):361-7.
(21.) Xiao O, Morgan IG, Ellwein LB, He M; Refractive Error Study in Children Study Group. Prevalence of Amblyopia in School-Aged Children and Variations by Age, Gender, and Ethnicity in a Multi-Country Refractive Error Study. Ophthalmology. 2015 Sep;122(9):1924-31. DOI 10.1016/j.ophtha.2015.05.034.
(22.) Colombia. Ministerio de Salud. Guía de práctica clínica para la prevención, la detección temprana, el diagnóstico, el tratamiento y el seguimiento de la ambliopía en menores de 18 años [Internet]. Bogotá: MinSalud; 2016 [citado 2016]. Disponible en: http://gpc.minsalud.gov.co/gpc_sites/Repositorio/Conv_637/GPC_ambliopia/gpc_ambliopia_completa.aspx
(23.) Lloyd IC, Ashworth J, Biswas S, Abadi RV. Advances in the management of congenital and infantile cataract. Eye (Lond). 2007 Oct;21(10):1301-9.DOI 10.1038/sj.eye.6702845.
(24.) Fan DS, Yip WW, Yu CB, Rao SK, Lam DS. Updates on the surgical management of paediatric cataract with primary intraocular lens implantation. Ann Acad Med Singapore. 2006 Aug;35(8):564-70.
(25.) Trumler AA. Evaluation of pediatric cataracts and systemic disorders. Curr Opin Ophthalmol. 2011 Sep;22(5):365-79. DOI 10.1097/ICU.0b013e32834994dc.
(26.) Moore DB, Tomkins O, Ben-Zion I. A review of primary congenital glaucoma in the developing world. Surv Ophthalmol. 2013 May-Jun;58(3):278-85. DOI 10.1016/j.survophthal.2012.11.003.
(27.) Majumder PD, Biswas J. Pediatric uveitis: An update. Oman J Ophthalmol. 2013 Sep;6(3):140-50. DOI 10.4103/0974-620X.122267.
(28.) Dimaras H, Kimani K, Dimba EA, Gronsdahl P, White A, Chan HS. Retinoblastoma. Lancet. 2012 Apr;379(9824):1436-46. DOI 10.1016/S0140-6736(11)61137-9.
(29.) Rodriguez-Galindo C, Orbach DB, VanderVeen D. Retinoblastoma. Pediatr Clin North Am. 2015 Feb;62(1):201-23. DOI 10.1016/j.pcl.2014.09.014.
(30.) Pandey AN. Retinoblastoma: An overview. Saudi J Ophthalmol. 2014 Oct;28(4):310-5. DOI 10.1016/j.sjopt.2013.11.001.
(31.) Committee on practice and ambulatory medicine on ophthalmology, American Association of Certified Orthoptists, American Association For Pediatric Ophthalmology and Strabismus, American academy of ophthalmology. Eye examination in infants, children and young adults by pediatricians. Ophthalmology. 2003;110(4):860-65. DOI 10.1016/S0161-6420(03)00414-7.
(32.) American Academy of Ophthalmology. Fundamentals and principles of ophthalmology 2017-2018. Section 2 [Internet]. San Francisco CA: BCSC;2017 [citado 2016]. Available from: file:///C:/Users/Informatica/Downloads/BCSC1718_S02.pdf
(33.) Powell C, Wedner S, Hatt SR. Vision screening for correctable visual acuity deficits in school-age children and adolescents. Cochrane Database Syst Rev. 2005;(4):CD005023. DOI 10.1002/14651858.CD005023.pub2.
(34.) Leat SJ, Yadav NK, Irving EL. Development of visual acuity and contrast sensitivity in children. J Optom. 2009;2(1):19-26. DOI 10.3921/joptom.2009.19.
(35.) Wright K. Ocular examination and vision screening. In: Pediatric Ophthalmology for Pediatricians. Baltimore: Williams & Wilkins; 1999. p. 39.
(36.) American Academy of Pediatrics Section on Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology, American Association of Certified Orthoptists. Policy Statement. Red reflex examination in neonates, infants, and children. Pediatrics. 2008;122(6):1401-4. DOI 10.1542/peds.2008-2624.
(37.) Dobson V, Clifford-Donaldson CE, Miller JM, Garvey KA, Harvey EM. A comparison of Lea Symbol vs ETDRS letter distance visual acuity in a population of young children with a high prevalence of astigmatism. J AAPOS. 2009 Jun;13(3):253-7. DOI 10.1016/j.jaapos.2009.01.007.
(38.) O’Neill S, McAndrew DJ. The validity of visual acuity assessment using mobile technology devices in the primary care setting. Aust Fam Physician. 2016 Apr;45(4):212-5.
(39.) Zhang ZT, Zhang SC, Huang XG, Liang LY. A pilot trial of the iPad tablet computer as a portable device for visual acuity testing. J Telemed Telecare. 2013 Jan;19(1):55-9. DOI 10.1177/1357633X12474964.
(40.) Taub MB. Comprehensive examination procedures. In Taub MB, Bartuccio M, Maino DM. Visual diagnosis and care of the patient with special needs. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2012. p. 157.
(41.) Morale SE, Hughbanks-Wheaton DK, Cheng C, Subramanian V, O’Connor AR, Birch EE. Visual acuity assessment of children with special needs. Am Orthopt J. 2012;62:90-8. DOI 10.3368/aoj.62.1.90.
(42.) Nielsen LS, Skov L, Jensen H. Visual dysfunctions and ocular disorders in children with developmental delay. I. prevalence, diagnoses and aetiology of visual impairment. Acta Ophthalmol Scand. 2007 Mar;85(2):149-56. DOI 10.1111/j.1600-0420.2006.00867.x.
(43.) Kozeis N, Anogeianaki A, Mitova DT, Anogianakis G, Mitov T, Klisarova A. Visual function and visual perception in cerebral palsied children. Ophthalmic Physiol Opt. 2007 Jan;27(1):44-53. DOI 10.1111/j.1475-1313.2006.00413.x
(44.) Friedman NJ, Kaiser PK. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 3ª ed. Barcelona: Elsevier, 2010.
(45.) Wilson FM, Blomquist PH. Ocular motility examination. In: Practical Ophthalmology: A manual for beginning residents. 6th ed. San Francisco CA: American Academy of Ophthalmology; 2009. p. 93-4.
(46.) Guerrero JJ. Optometría clínica. 2ª ed. Bogotá: Fundación Universitaria del Área Andina; 2012.
(47.) Childrens Eye Foundation. Amblyopia Economic Costs: Diminished Utility [Internet]. [cited 2018]. Available from: https://www.childrenseyefoundation.org/S/why-save-sight/economic-cost-of-failure-to-preventblindness-from-amblyopia/
(48.) Wittenborn J, Rein D. Cost of vision problems: The economic burden of vision loss and eye disorders in the United States. Chicago IL: NORC;2013 [cited 2013]. Available from: https://www.researchgate.net/publication/249960785_Cost_of_Vision_Problems_The_Economic_Burden_of_Vision_Loss_and_Eye_Disorders_in_the_United_States
(49.) Membreno JH, Brown MM, Brown GC, Sharma S, Beauchamp GR. A cost-utility analysis of therapy for amblyopia. Ophthalmology. 2002 Dec;109(12):2265-71.
(50.) Wallace DK, Repka MX, Lee KA, Melia M, Christiansen SP, Morse CL. Amblyopia Preferred Practice Pattern. Ophthalmology. 2018 Jan;125(1):105-42. DOI 10.1016/j.ophtha.2017.10.008.
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.