Anticholinergic load in patients older 65 years with ambulatory pharmacological treatment in a Colombian population
DOI:
https://doi.org/10.17533/udea.iatreia.v32n1a03Keywords:
anticholinergic syndrome, elderly, outpatients, polypharmacyAbstract
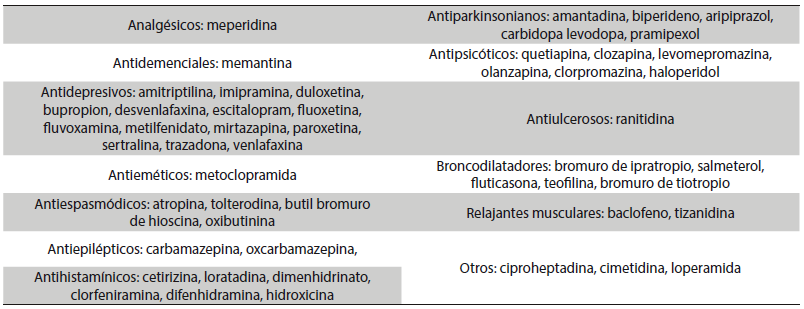
Background: Drugs with potential anticholinergic effect are usually prescribed to the population over 65 years. There are several scales created to calculate anticholinergic burden: Anticholinergic Drug Scale, Anticholinergic Risk Scale, and Anticholinergic Cognitive Burden.
Objective: To characterize the anticholinergic burden in patients older than 65 years with polypharmacy who are prescribed in ambulatory settings.
Methods: Retrospective cross-sectional study with information registered from April to September 2016. The database of prescription records of a health management organization (HMO), with national registries in the Pharmacy Benefit Management (PBM) technology platform, was used. Medicines were analyzed by its anticholinergic properties and anticholinergic burden.
Results: There were 115,713 patients with a median age of 74 years. The medicines with moderate anticholinergic burden were dimenhydrinate, amantadine, biperidene and quetiapine in 6.5 %, and with high anticholinergic burden hyoscine butylbromide and amitryptiline in 13.1 %.
Discussion: The medical attention of diseases of the elderly is complex and requires the prescription of multiple medications. It is important to evaluate the medicines and verify their relevance and possible pharmacological interactions, to avoid the presence of adverse events. For this reason, scales have been developed, they allow improving therapeutic results, and especially in medicines with anticholinergic burden and systems of clinical alerts that promotes correct formulation.
Downloads
References
(1.) Gavilan-Moral E, Villafaina-Barroso A, Jiménez-de Gracia L, Gómez Santana M del C. Ancianos frágiles polimedicados: ¿es la prescripción de medicamentos la salida? Rev Esp Geriatr Gerontol. 2012;47(4):137-86. DOI 10.1016/j.regg.2012.01.003.
(2.) Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017 Oct;17(1):230. DOI 10.1186/s12877-017-0621-2.
(3.) Laosa Zafra O, Tardáguila García N, Jordán Bueso J. Programas de farmacovigilancia en el anciano. En: Tratado de medicina geriátrica: Fundamentos de la atención sanitaria a los mayores. Ámsterdam: Elsevier; 2015. p. 56-65.
(4.) Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014 Jan;13(1):57-65. DOI 10.1517/14740338.2013.827660.
(5.) Moreno-Gutiérrez PA, Gaviria-Mendoza A, Cañón MM, Machado-Alba JE. High prevalence of risk factors in elderly patients using drugs associated with acquired torsades de pointes chronically in Colombia. Br J Clin Pharmacol. 2016 Aug;82(2):504-11. DOI 10.1111/bcp.12969.
(6.) Colombia. Ministerio de Salud. Informe quincenal epidemiológico nacional: Perfil epidemiológico de las intoxicaciones por sustancias químicas en Colombia, 2008-2015 [Internet]. Bogotá: MinSalud: 2017. Disponible en: https://www.ins.gov.co/buscador-eventos/IQEN/IQEN%20vol%2022%202017%20num%202.pdf
(7.) Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004 Jan;57(1):6-14.
(8.) Parekh N, Ali K, Stevenson JM, Davies JG, Schiff R, Van der Cammen T, et al. Incidence and cost of medication harm in older adults following hospital discharge: a multicenter prospective study in the UK. Br J Clin Pharmacol. 2018 Aug;84(8):1789-97. DOI 10.1111/bcp.13613.
(9.) Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev. 2009;41(2):67-76. DOI 10.1080/03602530902722679.
(10.) Salbu RL, Feuer J. A Closer Look at the 2015 Beers Criteria. J Pharm Pract. 2017 Aug;30(4):419-424. DOI 10.1177/0897190016663072.
(11.) American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015 Nov;63(11):2227-46. DOI 10.1111/jgs.13702.
(12.) O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015 Mar;44(2):213-8. DOI 10.1093/ageing/afu145.
(13.) Nauta KJ, Groenhof F, Schuling J, Hugtenburg JG, van Hout HPJ, Haaijer-Ruskamp FM, et al. Application of the STOPP/START criteria to a medical record database. Pharmacoepidemiol Drug Saf. 2017 Oct;26(10):1242-7. DOI 10.1002/pds.4283.
(14.) López-Álvarez J, Zea Sevilla MA, Agüera Ortiz L, Fernández Blázquez MÁ, Valentí Soler M, Martínez-Martín P. Efecto de los farmacos anticolinergicos en el rendimiento cognitivo de las personas mayores. Rev Psiquiatr Salud Ment. 2015;8(1):35-43.
(15.) Villalba-Moreno AM, Alfaro-Lara ER, Santos-Ramos B. Anticholinergic risk: Use and limitations of anticholinergic scales. Eur J Intern Med. 2015 Dec;26(10):e65-6. DOI 10.1016/j.ejim.2015.08.014.
(16.) Rojo-Sánchez AM, Vélez-Diaz-Pallares M, Muñoz García M, Delgado Silveira E, Bermejo Vicedo T, Cruz Jentoft A. Carga anticolinergica y delirium en pacientes mayores durante la hospitalizacion en una unidad de agudos de geriatría. Rev Esp Geriatr Gerontol. 2016;51(4):187-248. DOI 10.1016/j.regg.2016.04.004.
(17.) Naples JG, Marcum ZA, Perera S, Gray SL, Newman AB, Simonsick EM, et al. Concordance Between Anticholinergic Burden Scales. J Am Geriatr Soc. 2015 Oct;63(10):2120-4. DOI 10.1111/jgs.13647.
(18.) Carnahan RM, Lund BC, Perry PJ, Pollock BG, Culp KR. The Anticholinergic Drug Scale as a measure of drug-related anticholinergic burden: associations with serum anticholinergic activity. J Clin Pharmacol. 2006 Dec;46(12):1481-6.
(19.) Hsu WH, Wen YW, Chen LK, Hsiao FY. Comparative Associations Between Measures of Anti-cholinergic Burden and Adverse Clinical Outcomes. Ann Fam Med. 2017 Nov;15(6):561-9. DOI 10.1370/afm.2131.
(20.) Pont LG, Nielen JT, McLachlan AJ, Gnjidic D, Chan L, Cumming RG, et al. Measuring anticholinergic drug exposure in older community-dwelling Australian men: a comparison of four different measures. Br J Clin Pharmacol. 2015 Nov;80(5):1169-75. DOI 10.1111/bcp.12670.
(21.) Gorzoni ML, Alves Fabbri RM. Applicability of Anticholinergic Risk Scale in hospitalized elderly persons. Rev Bras Geriatr Gerontol. 2017;20(1):123-8. DOI 10.1590/1981-22562017020.150191.
(22.) Gray SL, Anderson ML, Dublin S, Hanlon JT, Hubbard R, Walker R, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015 Mar;175(3):401-7. DOI 10.1001/jamainternmed.2014.7663.
(23.) Mayer T, Kopitz J, Plaschke K, Weiss J, Seidling HM, Haefeli WE. Limitations of the Anticholinergic Activity Assay and Assay-Based Anticholinergic Drug Scales. Am J Geriatr Psychiatry. 2016 Dec;24(12):1182-8. DOI 10.1016/j.jagp.2016.07.024.
(24.) Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008 Mar;168(5):508-13. DOI 10.1001/archinternmed.2007.106.
(25.) Kose E, Hirai T, Seki T. Assessment of aspiration pneumonia using the Anticholinergic Risk Scale. Geriatr Gerontol Int. 2018:1230-5. DOI 10.1111/ggi.13454.
(26.) Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Patterns of drug use and factors associated with polypharmacy and excessive polypharmacy in elderly persons: results of the Kuopio 75+ study: a cross-sectional analysis. Drugs Aging. 2009;26(6):493-503. DOI 10.2165/00002512-200926060-00006.
(27.) Urfer M, Elzi L, Dell-Kuster S, Bassetti S. Intervention to Im Patients Admitted to an Internal Medicine Unit. PLoS One. 2016 Nov;11(11):e0166359. DOI 10.1371/journal.pone.0166359.
(28.) Shah BM, Hajjar ER. Polypharmacy, adverse drug reactions, and geriatric syndromes. Clin Geriatr Med. 2012 May;28(2):173-86. DOI 10.1016/j.cger.2012.01.002.
(29.) Salahudeen MS, Hilmer SN, Nishtala PS. Comparison of anticholinergic risk scales and associations with adverse health outcomes in older people. J Am Geriatr Soc. 2015 Jan;63(1):85-90. DOI 10.1111/jgs.13206.
(30.) Villalba-Moreno AM, Alfaro-Lara ER, Pérez-Guerrero MC, Nieto-Martín MD, Santos-Ramos B. Systematic review on the use of anticholinergic scales in poly pathological patients. Arch Gerontol Geriatr. 2016 Jan-Feb;62:1-8. DOI 10.1016/j.archger.2015.10.002. Erratum in: Arch Gerontol Geriatr. 2016 May-Jun;64:178-80.
(31.) Lertxundi U, Domingo-Echaburu S, Hernandez R, Peral J, Medrano J. Expert-based drug lists to measure anticholinergic burden: similar names, different results. Psychogeriatrics. 2013 Mar;13(1):17-24. DOI 10.1111/j.1479-8301.2012.00418.x.
(32.) Narayan SW, Hilmer SN, Horsburgh S, Nishtala PS. Anticholinergic component of the Drug Burden Index and the Anticholinergic Drug Scale as measures of anticholinergic exposure in older people in New Zealand: a population-level study. Drugs Aging. 2013 Nov;30(11):927-34. DOI 10.1007/s40266-013-0111-y.
(33.) West T, Pruchnicki MC, Porter K, Emptage R. Evaluation of anticholinergic burden of medications in older adults. J Am Pharm Assoc (2003). 2013 Sep-Oct;53(5):496-504. DOI 10.1331/JAPhA.2013.12138.
(34.) Tisdale JE. Drug-induced QT interval prolongation and torsades de pointes: Role of the pharmacist in risk assessment, prevention and management. Can Pharm J (Ott). 2016 May;149(3):139-52. DOI 10.1177/1715163516641136.
(35.) Khan Q, Ismail M, Haider I, Ali Z. Prevalence of the risk factors for QT prolongation and associated drug-drug interactions in a cohort of medical inpatients. J Formos Med Assoc. 2018 Feb. pii: S0929-6646(17)30607-1. DOI 10.1016/j.jfma.2018.01.016.
(36.) World Health Organization. Clinical pharmacology in health care, teaching and research [Internet]. Geneva, Switzerland: WHO; 2012. Available from: http://apps.who.int/medicinedocs/documents/s19916en/s19916en.pdf
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.