Chronic mucocutaneous candidiasis: a look at genetic understanding
DOI:
https://doi.org/10.17533/udea.%20iatreia.v31n4a06Keywords:
autoimmune polyendocrinopathy, chronic mucocutaneous candidiasis , factor de transcripción STAT1, geneticsAbstract
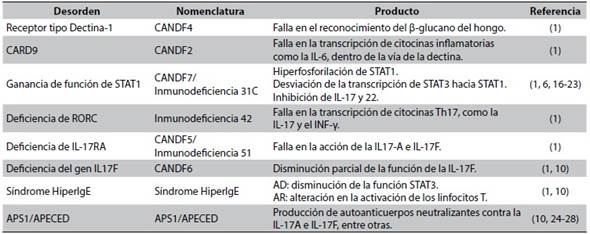
Chronic mucocutaneous candidiasis is an infectious phenotype characterized by recurrent or persistent infections in the skin, nails and mucous membranes produced by Candida sp. This is secondary to any alteration in the antifungal immunity, in which not only the production of IL-17, but any defect in the differentiation of the T lymphocytes towards their TH17 profile, play a fundamental role and will unchain a susceptibility to this infection; that depending on the genetic etiology, can be a syndromic manifestation with other associated infectious and endocrinological clinical characteristics. Here, we review in a practical, clear and concise manner, the genetic defects so far found to be involved in the appearance of chronic mucocutaneous candidiasis.
Downloads
References
(1.) Green L, Dolen WK. Chronic Candidiasis in Children. Curr Allergy Asthma Rep.2017 May;17(5):31. DOI 10.1007/s11882-017-0699-9.
(2.) Reyes Delgado K, Staines Boone AT, Amaya Guerra M, González Cabello D, García Campos J, Sánchez Sánchez LM, et al. Candidiasis mucocutánea crónica. Dermatol Rev Mex. 2013;57(5):378-81.
(3.) Dotta L, Scomodon O, Padoan R, Timpano S, Plebani A, Soresina A, et al. Clinical and immunological data of nine patients with chronic mucocutaneous candidiasis disease. Data Brief. 2016 Feb;7:311-5. DOI 10.1016/j.dib.2016.02.040.
(4.) Wang Q, Dufresne SF, Vinh DC, Aubin MJ. Chronic mucocutaneous candidiasis presenting as Candida endophthalmitis. Can J Ophthalmol. 2016 Apr;51(2):e55-8. DOI 10.1016/j.jcjo.2015.11.004.
(5.) Khullar G, Vignesh P, Lau YL, Rudramurthy SM, Rawat A, De D, et al. Chronic Mucocutaneous Candidiasis. J Allergy Clin Immunol Pract. 2017 Jul-Aug;5(4):1119-21. DOI 10.1016/j.jaip.2016.11.025.
(6.) Nielsen J, Kofod-Olsen E, Spaun E, Larsen CS, Christiansen M, Mogensen TH. A STAT1-gain-of-function mutation causing Th17 deficiency with chronic mucocutaneous candidiasis, psoriasiform hyperkeratosis and dermatophytosis. BMJ Case Rep. 2015 Oct;2015. pii: bcr2015211372. DOI 10.1136/bcr-2015-211372. Erratum in: BMJ Case Rep. 2015;2015. pii: bcr-2015211372corr1. DOI 10.1136/bcr-2015-211372corr1.
(7.) Herrod HG. Chronic mucocutaneous candidiasis in childhood and complications of non-Candida infection: a report of the Pediatric Immunodeficiency Collaborative Study Group. J Pediatr. 1990 Mar;116(3):377-82.
(8.) Eyerich K, Eyerich S, Hiller J, Behrendt H, Traidl-Hoffmann C. Chronic mucocutaneous candidiasis, from bench to bedside. Eur J Dermatol. 2010 May-Jun;20(3):260-5. DOI 10.1684/ejd.2010.0910.
(9.) Taylor PR, Tsoni SV, Willment JA, Dennehy KM, Rosas M, Findon H, et al. Dectin-1 is required for beta-glucan recognition and control of fungal infection. Nat Immunol. 2007 Jan;8(1):31-8.
(10.) Huppler AR, Bishu S, Gaffen SL. Mucocutaneous candidiasis: the IL-17 pathway and implications for targeted immunotherapy. Arthritis Res Ther. 2012 Jul;14(4):217. DOI 10.1186/ar3893.
(11.) Pfaller MA, Diekema DJ, Gibbs DL, Newell VA, Ellis D, Tullio V, et al. Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: a 10.5-year analysis of susceptibilities of Candida Species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. J Clin Microbiol. 2010 Apr;48(4):1366-77. DOI 10.1128/JCM.02117-09.
(12.) Firinu D, Massidda O, Lorrai MM, Serusi L, Peralta M, Barca MP, et al. Successful treatment of chronic mucocutaneous candidiasis caused by azole-resistant Candida albicans with posaconazole. Clin Dev Immunol. 2011;2011:283239. DOI 10.1155/2011/283239.
(13.) Rautemaa R, Richardson M, Pfaller MA, Perheentupa J, Saxén H. Activity of amphotericin B, anidulafungin, caspofungin, micafungin, posaconazole, and voriconazole against Candida albicans with decreased susceptibility to fluconazole from APECED patients on long-term azole treatment of chronic mucocutaneous candidiasis. Diagn Microbiol Infect
Dis. 2008 Oct;62(2):182-5. DOI 10.1016/j.diagmicrobio.2008.05.007.
(14.) Higgins E, Al Shehri T, McAleer MA, Conlon N, Feighery C, Lilic D, et al. Use of ruxolitinib to successfully treat chronic mucocutaneous candidiasis caused by gain-of-function signal transducer and activator of transcription 1 (STAT1) mutation. J Allergy Clin Immunol. 2015 Feb;135(2):551-3. DOI 10.1016/j.jaci.2014.12.1867.
(15.) van de Veerdonk FL, Netea MG. Treatment options for chronic mucocutaneous candidiasis. J Infect. 2016 Jul;72 Suppl:S56-60. DOI 10.1016/j.jinf.2016.04.023.
(16.) Okada S, Puel A, Casanova JL, Kobayashi M. Chronic mucocutaneous candidiasis disease associated with inborn errors of IL-17 immunity. Clin Transl Immunology. 2016 Dec;5(12):e114. DOI 10.1038/cti.2016.71.
(17.) Takezaki S, Yamada M, Kato M, Park MJ, Maruyama K, Yamazaki Y, et al. Chronic mucocutaneous candidiasis caused by a gain-of-function mutation in the STAT1 DNA-binding domain. J Immunol. 2012 Aug;189(3):1521-6. DOI 10.4049/jimmunol.1200926.
(18.) Martinez-Martinez L, Martinez-Saavedra MT, Fuentes-Prior P, Barnadas M, Rubiales MV, Noda J, et al. A novel gain-of-function STAT1 mutation resulting in basal phosphorylation of STAT1 and increased distal IFN-γ-mediated responses in chronic mucocutaneous candidiasis. Mol Immunol. 2015 Dec;68(2 Pt C):597-605. DOI 10.1016/j.molimm.2015.09.014.
(19.) Zheng J, van de Veerdonk FL, Crossland KL, Smeekens SP, Chan CM, Al Shehri T, et al. Gain-of-function STAT1 mutations impair STAT3 activity in patients with chronic mucocutaneous candidiasis (CMC). Eur J Immunol. 2015 Oct;45(10):2834-46. DOI 10.1002/eji.201445344.
(20.) Wang X, Zhang R, Wu W, Wang A, Wan Z, van de Veerdonk FL, et al. New and recurrent STAT1 mutations in seven Chinese patients with chronic mucocutaneous candidiasis. Int J Dermatol. 2017 Feb;56(2):e30-e33. DOI 10.1111/ijd.13427.
(21.) Dotta L, Scomodon O, Padoan R, Timpano S, Plebani A, Soresina A, et al. Clinical heterogeneity of dominant chronic mucocutaneous candidiasis disease: presenting as treatment-resistant candidiasis and chronic lung disease. Clin Immunol. 2016 Mar;164:1-9. DOI 10.1016/j.clim.2015.12.010.
(22.) van de Veerdonk FL, Plantinga TS, Hoischen A, Smeekens SP, Joosten LA, Gilissen C, et al. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N Engl J Med. 2011 Jul;365(1):54-61. DOI 10.1056/NEJMoa1100102.
(23.) Dhalla F, Fox H, Davenport EE, Sadler R, Anzilotti C, van Schouwenburg PA, et al. Chronic mucocutaneous candidiasis: characterization of a family with STAT-1 gain-of-function and development of an ex-vivo assay for Th17 deficiency of diagnostic utility. Clin Exp Immunol. 2016 May;184(2):216-27. DOI 10.1111/cei.12746.
(24.) Finnish-German APECED Consortium. An autoimmune disease, APECED, caused by mutations in a novel gene featuring two PHD-type zinc-finger domains. Nat Genet. 1997 Dec;17(4):399-403.
(25.) Puel A, Döffinger R, Natividad A, Chrabieh M, Barcenas-Morales G, Picard C, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med. 2010 Feb;207(2):291-7. DOI 10.1084/jem.20091983.
(26.) Sarkadi AK, Taskó S, Csorba G, Tóth B, Erdős M, Maródi L. Autoantibodies to IL-17A may be correlated with the severity of mucocutaneous candidiasis in APECED patients. J Clin Immunol. 2014 Feb;34(2):181-93. DOI 10.1007/s10875-014-9987-5.
(27.) Pedroza LA, Kumar V, Sanborn KB, Mace EM, Niinikoski H, Nadeau K, et al. Autoimmune regulator (AIRE) contributes to Dectin-1-induced TNF-α production and complexes with caspase recruitment domain-containing protein 9 (CARD9), spleen tyrosine kinase (Syk), and Dectin-1. J Allergy Clin Immunol. 2012 Feb;129(2):464-72, 472.e1-3. DOI 10.1016/j.jaci.2011.08.027.
(28.) Capalbo D, Improda N, Esposito A, De Martino L, Barbieri F, Betterle C, et al. Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy from the pediatric perspective. J Endocrinol Invest. 2013 Nov;36(10):903-12. DOi 10.3275/8999.
(29.) Kalfa VC, Roberts RL, Stiehm ER. The syndrome of chronic mucocutaneous candidiasis with selective antibody deficiency. Ann Allergy Asthma Immunol. 2003 Feb;90(2):259-64.
Published
How to Cite
Issue
Section
License
Copyright (c) 2018 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.