Inflamación y respuesta inmune innata: participación de las lipoproteínas de alta densidad
DOI:
https://doi.org/10.17533/udea.iatreia.v30n4a06Palabras clave:
colesterol, HDL, inmunomodulación, respuesta inmuneResumen
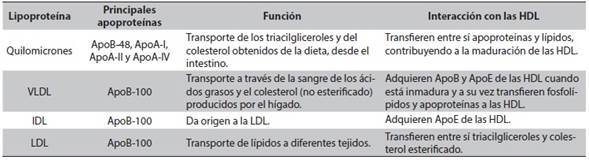
Las lipoproteínas de alta densidad (HDL) tienen como función transportar el exceso de colesterol desde los tejidos hacia el hígado, para ser excretado; y de este modo contribuyen al control de las enfermedades cardiovasculares. Además, las HDL pueden modular la respuesta inmune, por sus propiedades anti-inflamatorias, antioxidantes y anti-apoptóticas, entre otras. A nivel celular, las HDL pueden modificar las balsas lipídicas, las cuales son determinantes en la activación de la respuesta inmune frente a patógenos o agentes extraños. En algunas patologías como la sepsis, las HDL participan mediando la eliminación del lipopolisacárido (LPS) a través de su captura y posterior eliminación en el hígado; esto conlleva a una modulación negativa de la expresión del TLR4, principal receptor del LPS. También se ha reportado que las HDL modulan la respuesta inflamatoria a través de la regulación de la activación de la cascada del complemento y la expresión de pentraxina 3. Finalmente, la función y los niveles de las HDL se han encontrado particularmente alterados en algunas patologías infecciosas, ateroesclerosis y sepsis, lo que se ha asociado con el progreso o la severidad de la enfermedad.
Descargas
Citas
(1.) Feingold KR, Grunfeld C. Introduction to Lipids and Lipoproteins. In: De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000 [cited 2017 Mar]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK305896/
(2.) Li XA, Titlow WB, Jackson BA, Giltiay N, Nikolova-Karakashian M, Uittenbogaard A, et al. High density lipoprotein binding to scavenger receptor, Class B, type I activates endothelial nitric-oxide synthase in a ceramide-dependent manner. J Biol Chem. 2002 Mar;277(13):11058-63. DOI 10.1074/jbc.M110985200.
(3.) Uittenbogaard A, Shaul PW, Yuhanna IS, Blair A, Smart EJ. High density lipoprotein prevents oxidized low density lipoprotein-induced inhibition of endothelial nitric-oxide synthase localization and activation in caveolae. J Biol Chem. 2000 Apr;275(15):11278-83.
(4.) Kameda T, Ohkawa R, Yano K, Usami Y, Miyazaki A, Matsuda K, et al. Effects of Myeloperoxidase-Induced Oxidation on Antiatherogenic Functions of High-Density Lipoprotein. J Lipids. 2015;2015:592594. DOI 10.1155/2015/592594.
(5.) Nofer JR, Levkau B, Wolinska I, Junker R, Fobker M, von Eckardstein A, et al. Suppression of endothelial cell apoptosis by high density lipoproteins (HDL) and HDL-associated lysosphingolipids. J Biol Chem. 2001 Sep;276(37):34480-5. DOI 10.1074/jbc.M103782200.
(6.) Zhu X, Owen JS, Wilson MD, Li H, Griffiths GL, Thomas MJ, et al. Macrophage ABCA1 reduces MyD88-dependent Toll-like receptor trafficking to lipid rafts by reduction of lipid raft cholesterol. J Lipid Res. 2010 Nov;51(11):3196-206. DOI 10.1194/jlr.M006486.
(7.) Chowdhury SM, Zhu X, Aloor JJ, Azzam KM, Gabor KA, Ge W, et al. Proteomic Analysis of ABCA1-Null Macrophages Reveals a Role for Stomatin-Like Protein-2 in Raft Composition and Toll-Like Receptor Signaling. Mol Cell Proteomics. 2015 Jul;14(7):1859-70. DOI 10.1074/mcp.M114.045179.
(8.) Simons K, Toomre D. Lipid rafts and signal transduction. Nat Rev Mol Cell Biol. 2000 Oct;1(1):31-9. Erratum in: Nat Rev Mol Cell Biol 2001 Mar;2(3):216. DOI 10.1038/35036052.
(9.) Kapadia SB, Barth H, Baumert T, McKeating JA, Chisari FV. Initiation of hepatitis C virus infection is dependent on cholesterol and cooperativity between CD81 and scavenger receptor B type I. J Virol. 2007 Jan;81(1):374-83. DOI 10.1128/JVI.01134-06.
(10.) Vaisar T, Pennathur S, Green PS, Gharib SA, Hoofnagle AN, Cheung MC, et al. Shotgun proteomics implicates protease inhibition and complement activation in the anti-inflammatory properties of HDL. J Clin Invest. 2007 Mar;117(3):746-56. DOI 10.1172/JCI26206.
(11.) Niculescu LS, Simionescu N, Sanda GM, Carnuta MG, Stancu CS, Popescu AC, et al. MiR-486 and miR-92a Identified in Circulating HDL Discriminate between Stable and Vulnerable Coronary Artery Disease Patients. PLoS One. 2015 Oct;10(10):e0140958. DOI 10.1371/journal.pone.0140958.
(12.) Vickers KC, Palmisano BT, Shoucri BM, Shamburek RD, Remaley AT. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol. 2011 Apr;13(4):423-33. DOI 10.1038/ncb2210. Erratum in: Nat Cell Biol. 2015 Jan;17(1):104.
(13.) Gidez LI, Miller GJ, Burstein M, Slagle S, Eder HA. Separation and quantitation of subclasses of human plasma high density lipoproteins by a simple precipitation procedure. J Lipid Res. 1982 Nov;23(8):1206-23.
(14.) Gu X, Kozarsky K, Krieger M. Scavenger receptor class B, type I-mediated [3H]cholesterol efflux to high and low density lipoproteins is dependent on lipoprotein binding to the receptor. J Biol Chem. 2000 Sep;275(39):29993-30001.
(15.) Asztalos BF, de la Llera-Moya M, Dallal GE, Horvath KV, Schaefer EJ, Rothblat GH. Differential effects of HDL subpopulations on cellular ABCA1- and SRBI-mediated cholesterol efflux. J Lipid Res. 2005 Oct;46(10):2246-53. DOI 10.1194/jlr.M500187-JLR200.
(16.) Clay MA, Pyle DH, Rye KA, Barter PJ. Formation of spherical, reconstituted high density lipoproteins containing both apolipoproteins A-I and A-II is mediated by lecithin:cholesterol acyltransferase. J Biol Chem. 2000 Mar;275(12):9019-25.
(17.) Asztalos BF, Schaefer EJ, Horvath KV, Yamashita S, Miller M, Franceschini G, et al. Role of LCAT in HDL remodeling: investigation of LCAT deficiency states. J Lipid Res. 2007 Mar;48(3):592-9. DOI 10.1194/jlr.M600403-JLR200.
(18.) Acton S, Rigotti A, Landschulz KT, Xu S, Hobbs HH, Krieger M. Identification of scavenger receptor SR-BI as a high density lipoprotein receptor. Science. 1996 Jan;271(5248):518-20.
(19.) Hesler CB, Tall AR, Swenson TL, Weech PK, Marcel YL, Milne RW. Monoclonal antibodies to the Mr 74,000 cholesteryl ester transfer protein neutralize all of the cholesteryl ester and triglyceride transfer activities in human plasma. J Biol Chem. 1988 Apr;263(11):5020-3.
(20.) Tape C, Kisilevsky R. Apolipoprotein A-I and apolipoprotein SAA half-lives during acute inflammation and amyloidogenesis. Biochim Biophys Acta. 1990 Apr;1043(3):295-300.
(21.) Han CY, Tang C, Guevara ME, Wei H, Wietecha T, Shao B, et al. Serum amyloid A impairs the antiinflammatory properties of HDL. J Clin Invest. 2016 Jan;126(1):266-81. DOI 10.1172/JCI83475. Erratum in: J Clin Invest. 2016 Feb;126(2):796.
(22.) Pussinen PJ, Metso J, Malle E, Barlage S, Palosuo T, Sattler W, et al. The role of plasma phospholipid transfer protein (PLTP) in HDL remodeling in acute-phase patients. Biochim Biophys Acta. 2001 Sep;1533(2):153-63.
(23.) Sprandel MC, Hueb WA, Segre A, Ramires JA, Kalil-Filho R, Maranhão RC. Alterations in lipid transfers to HDL associated with the presence of coronary artery disease in patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2015 Aug;14:107. DOI 10.1186/s12933-015-0270-8.
(24.) Hernandez JC, Sirois CM, Latz E. Activation and regulation of the NLRP3 inflammasome. In: Couillin I, Pétrilli V, Martinon F, editors. The Inflammasomes. Berlin: Springer Basel; 2011. p. 197-208. DOI 10.1007/978-3-0348-0148-5_13.
(25.) Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterolcrystals. Nature. 2010 Apr;464(7293):1357-61. DOI 10.1038/nature08938. Erratum in: Nature. 2010 Jul;466(7306):652.
(26.) Rajamäki K, Lappalainen J, Oörni K, Välimäki E, Matikainen S, Kovanen PT, et al. Cholesterol crystals activate the NLRP3 inflammasome in human macrophages: a novel link between cholesterol metabolism and inflammation. PLoS One. 2010 Jul;5(7):e11765. DOI 10.1371/journal.pone.0011765.
(27.) Thacker SG, Zarzour A, Chen Y, Alcicek MS, Freeman LA, Sviridov DO, et al. High-density lipoprotein reduces inflammation from cholesterol crystals by inhibiting inflammasome activation. Immunology. 2016 Nov;149(3):306-19. DOI 10.1111/imm.12638.
(28.) Zheng F, Xing S, Gong Z, Mu W, Xing Q. Silence of NLRP3 suppresses atherosclerosis and stabilizes plaques in apolipoprotein E-deficient mice. Mediators Inflamm. 2014;2014:507208. DOI 10.1155/2014/507208.
(29.) Whitman SC, Ravisankar P, Daugherty A. Interleukin-18 enhances atherosclerosis in apolipoprotein E(-/-) mice through release of interferon-gamma. Circ Res. 2002 Feb;90(2):E34-8.
(30.) Kellner-Weibel G, Yancey PG, Jerome WG, Walser T, Mason RP, Phillips MC, et al. Crystallization of free cholesterol in model macrophage foam cells. Arterioscler Thromb Vasc Biol. 1999 Aug;19(8):1891-8.
(31.) Wang L, Qu P, Zhao J, Chang Y. NLRP3 and downstream cytokine expression elevated in the monocytes of patients with coronary artery disease. Arch Med Sci. 2014 Aug;10(4):791-800. DOI 10.5114/aoms.2014.44871.
(32.) Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977 May;62(5):707-14.
(33.) Harel M, Aharoni A, Gaidukov L, Brumshtein B, Khersonsky O, Meged R, et al. Structure and evolution of the serum paraoxonase family of detoxifying and anti-atherosclerotic enzymes. Nat Struct Mol Biol. 2004 May;11(5):412-9. Erratum in: Nat Struct Mol Biol. 2004 Dec;11(12):1253. DOI 10.1038/nsmb767.
(34.) Bounafaa A, Berrougui H, Ghalim N, Nasser B, Bagri A, Moujahid A, et al. Association between Paraoxonase 1 (PON1) Polymorphisms and the Risk of Acute Coronary Syndrome in a North African Population. PLoS One. 2015 Aug;10(8):e0133719. DOI 10.1371/journal.pone.0133719.
(35.) Sanguinetti SM, Brites FD, Fasulo V, Verona J, Elbert A, Wikinski RL, Schreier LE. HDL oxidability and its protective effect against LDL oxidation in Type 2 diabetic patients. Diabetes Nutr Metab. 2001 Feb;14(1):27-36.
(36.) Rozenberg O, Rosenblat M, Coleman R, Shih DM, Aviram M. Paraoxonase (PON1) deficiency is associated with increased macrophage oxidative stress: studies in PON1-knockout mice. Free Radic Biol Med. 2003 Mar;34(6):774-84.
(37.) Henning MF, Herlax V, Bakás L. Contribution of the C-terminal end of apolipoprotein AI to neutralization of lipopolysaccharide endotoxic effect. Innate Immun. 2011 Feb;17(3):327-37. DOI 10.1177/1753425910370709.
(38.) Hoshino K, Takeuchi O, Kawai T, Sanjo H, Ogawa T, Takeda Y, et al. Cutting edge: Toll-like receptor 4 (TLR4)-deficient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J Immunol. 1999 Apr;162(7):3749-52.
(39.) Guo L, Ai J, Zheng Z, Howatt DA, Daugherty A, Huang B, et al. High density lipoprotein protects against polymicrobe-induced sepsis in mice. J Biol Chem. 2013 Jun;288(25):17947-53. DOI 10.1074/jbc.M112.442699.
(40.) Levine DM, Parker TS, Donnelly TM, Walsh A, Rubin AL. In vivo protection against endotoxin by plasma high density lipoprotein. Proc Natl Acad Sci U S A. 1993 Dec;90(24):12040-4.
(41.) Gegner JA, Ulevitch RJ, Tobias PS. Lipopolysaccharide (LPS) signal transduction and clearance. Dual roles for LPS binding protein and membrane CD14. J Biol Chem. 1995 Mar;270(10):5320-5.
(42.) Levels JH, Marquart JA, Abraham PR, van den Ende AE, Molhuizen HO, van Deventer SJ, et al. Lipopolysaccharide is transferred from high-density to low-density lipoproteins by lipopolysaccharidebinding protein and phospholipid transfer protein. Infect Immun. 2005 Apr;73(4):2321-6. DOI 10.1128/IAI.73.4.2321-2326.2005.
(43.) Casas AT, Hubsch AP, Rogers BC, Doran JE. Reconstituted high-density lipoprotein reduces LPS-stimulated TNF alpha. J Surg Res. 1995 Nov;59(5):544-52. DOI 10.1006/jsre.1995.1204.
(44.) Guo L, Song Z, Li M, Wu Q, Wang D, Feng H, et al. Scavenger Receptor BI Protects against Septic Death through Its Role in Modulating Inflammatory Response. J Biol Chem. 2009 Jul;284(30):19826-34. DOI
1074/jbc.M109.020933.
(45.) Gilibert S, Galle-Treger L, Moreau M, Saint-Charles F, Costa S, Ballaire R, et al. Adrenocortical scavenger receptor class B type I deficiency exacerbates endotoxic shock and precipitates sepsis-induced mortality in mice. J Immunol. 2014 Jul;193(2):817-26. DOI 10.4049/jimmunol.1303164.
(46.) Smythies LE, White CR, Maheshwari A, Palgunachari MN, Anantharamaiah GM, Chaddha M, et al. Apolipoprotein A-I mimetic 4F alters the function of human monocyte-derived macrophages. Am J Physiol Cell Physiol. 2010 Jun;298(6):C1538-48. DOI 10.1152/ajpcell.00467.2009.
(47.) Khovidhunkit W, Kim MS, Memon RA, Shigenaga JK, Moser AH, Feingold KR, et al. Effects of infection and inflammation on lipid and lipoprotein metabolism: mechanisms and consequences to the host. J Lipid Res. 2004 Jul;45(7):1169-96.
(48.) Murphy AJ, Woollard KJ, Suhartoyo A, Stirzaker RA, Shaw J, Sviridov D, et al. Neutrophil activation is attenuated by high-density lipoprotein and apolipoprotein A-I in in vitro and in vivo models of inflammation. Arterioscler Thromb Vasc Biol. 2011 Jun;31(6):1333-41. DOI 10.1161/ATVBAHA.111.226258.
(49.) Murphy AJ, Woollard KJ, Hoang A, Mukhamedova N, Stirzaker RA, McCormick SP, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008 Nov;28(11):2071-7. DOI 10.1161/ATVBAHA.108.168690.
(50.) Manna PR, Sennoune SR, Martinez-Zaguilan R, Slominski AT, Pruitt K. Regulation of retinoid mediated cholesterol efflux involves liver X receptor activation in mouse macrophages. Biochem Biophys Res Commun. 2015 Aug;464(1):312-7. DOI 10.1016/j.bbrc.2015.06.150.
(51.) Castrillo A, Joseph SB, Vaidya SA, Haberland M, Fogelman AM, Cheng G, et al. Crosstalk between LXR and toll-like receptor signaling mediates bacterial and viral antagonism of cholesterol metabolism. Mol Cell. 2003 Oct;12(4):805-16.
(52.) Moudry R, Spycher MO, Doran JE. Reconstituted high density lipoprotein modulates adherence of polymorphonuclear leukocytes to human endothelial cells. Shock. 1997 Mar;7(3):175-81.
(53.) Kabouridis PS, Janzen J, Magee AL, Ley SC. Cholesterol depletion disrupts lipid rafts and modulates the activity of multiple signaling pathways in T lymphocytes. Eur J Immunol. 2000 Mar;30(3):954-63. DOI 10.1002/1521-141(200003)30:3<954::AIDIMMU954>3.0.CO;2-Y.
(54.) Hiltbold EM, Poloso NJ, Roche PA. MHC class IIpeptide complexes and APC lipid rafts accumulate at the immunological synapse. J Immunol. 2003 Feb;170(3):1329-38.
(55.) Wang SH, Yuan SG, Peng DQ, Zhao SP. HDL and ApoA-I inhibit antigen presentation-mediated T cell activation by disrupting lipid rafts in antigen presenting cells. Atherosclerosis. 2012 Nov;225(1):105-14. DOI 10.1016/j.atherosclerosis.2012.07.029.
(56.) Kim KD, Lim HY, Lee HG, Yoon DY, Choe YK, Choi I, et al. Apolipoprotein A-I induces IL-10 and PGE2 production in human monocytes and inhibits dendritic cell differentiation and maturation. Biochem Biophys Res Commun. 2005 Dec;338(2):1126-36.
(57.) Xu XH, Shah PK, Faure E, Equils O, Thomas L, Fishbein MC, et al. Toll-like receptor-4 is expressed by macrophages in murine and human lipid-rich atherosclerotic plaques and upregulated by oxidized LDL. Circulation. 2001 Dec 18;104(25):3103-8.
(58.) Triantafilou M, Triantafilou K. Receptor cluster formation during activation by bacterial products. J Endotoxin Res. 2003;9(5):331-5. DOI 10.1179/096805103225002557.
(59.) White CR, Smythies LE, Crossman DK, Palgunachari MN, Anantharamaiah GM, Datta G. Regulation of pattern recognition receptors by the apolipoprotein A-I mimetic peptide 4F. Arterioscler Thromb Vasc Biol. 2012 Nov;32(11):2631-9. DOI 10.1161/ATVBAHA.112.300167.
(60.) De Nardo D, Labzin LI, Kono H, Seki R, Schmidt SV, Beyer M, et al. High-density lipoprotein mediates anti-inflammatory reprogramming of macrophages via the transcriptional regulator ATF3. Nat Immunol. 2014 Feb;15(2):152-60. DOI 10.1038/ni.2784.
(61.) Scanu AM, Edelstein C. HDL: bridging past and present with a look at the future. FASEB J. 2008 Dec;22(12):4044-54. DOI 10.1096/fj.08-117150.
(62.) Olivera A, Kohama T, Edsall L, Nava V, Cuvillier O, Poulton S, et al. Sphingosine kinase expression increases intracellular sphingosine-1-phosphate and promotes cell growth and survival. J Cell Biol. 1999 Nov;147(3):545-58.
(63.) Mattie M, Brooker G, Spiegel S. Sphingosine-1-phosphate, a putative second messenger, mobilizes calcium from internal stores via an inositol trisphosphate-independent pathway. J Biol Chem. 1994 Feb;269(5):3181-8.
(64.) Li X, Stankovic M, Bonder CS, Hahn CN, Parsons M, Pitson SM, et al. Basal and angiopoietin-1-mediated endothelial permeability is regulated by sphingosine kinase-1. Blood. 2008 Apr;111(7):3489-97. DOI 10.1182/blood-2007-05-092148.
(65.) Samy ET, Meyer CA, Caplazi P, Langrish CL, Lora JM, Bluethmann H, et al. Cutting edge: Modulation of intestinal autoimmunity and IL-2 signaling by sphingosine kinase 2 independent of sphingosine 1-phosphate. J Immunol. 2007 Nov;179(9):5644-8.
(66.) Teijaro JR, Walsh KB, Cahalan S, Fremgen DM, Roberts E, Scott F, et al. Endothelial cells are central orchestrators of cytokine amplification during influenza virus infection. Cell. 2011 Sep;146(6):980-91. DOI 10.1016/j.cell.2011.08.015.
(67.) Oskeritzian CA, Alvarez SE, Hait NC, Price MM, Milstien S, Spiegel S. Distinct roles of sphingosine kinases 1 and 2 in human mast-cell functions. Blood. 2008 Apr;111(8):4193-200. DOI 10.1182/blood-2007-09-115451.
(68.) Zhang B, Tomura H, Kuwabara A, Kimura T, Miura S, Noda K, et al. Correlation of high density lipoprotein (HDL)-associated sphingosine 1-phosphate with serum levels of HDL-cholesterol and apolipoproteins. Atherosclerosis. 2005 Jan;178(1):199-205. DOI 10.1016/j.atherosclerosis.2004.08.024.
(69.) Liu M, Allegood J, Zhu X, Seo J, Gebre AK, Boudyguina E, et al. Uncleaved ApoM signal peptide is required for formation of large ApoM/sphingosine 1-phosphate (S1P)-enriched HDL particles. J Biol Chem. 2015 Mar;290(12):7861-70. DOI 10.1074/jbc.M114.631101.
(70.) Kimura T, Tomura H, Mogi C, Kuwabara A, Damirin A, Ishizuka T, et al. Role of scavenger receptor class B type I and sphingosine 1-phosphate receptors in high density lipoprotein-induced inhibition of adhesion molecule expression in endothelial cells. J Biol Chem. 2006 Dec;281(49):37457-67. DOI 10.1074/jbc.M605823200.
(71.) Pasqui AL, Puccetti L, Bova G, Di Renzo M, Bruni F, Pastorelli M, et al. Relationship between serum complement and different lipid disorders. Clin Exp Med. 2002 May;2(1):33-8.
(72.) Jenne DE, Lowin B, Peitsch MC, Böttcher A, Schmitz G, Tschopp J. Clusterin (complement lysis inhibitor) forms a high density lipoprotein complex with apolipoprotein A-I in human plasma. J Biol Chem. 1991 Jun;266(17):11030-6.
(73.) Speidl WS, Kastl SP, Huber K, Wojta J. Complement in atherosclerosis: friend or foe? J Thromb Haemost. 2011 Mar;9(3):428-40. DOI 10.1111/j.1538-7836.2010.04172.x.
(74.) Niyonzima N, Samstad EO, Aune MH, Ryan L, Bakke SS, Rokstad AM, et al. Reconstituted High-Density Lipoprotein Attenuates Cholesterol Crystal-Induced Inflammatory Responses by Reducing Complement Activation. J Immunol. 2015 Jul;195(1):257-64. DOI 10.4049/jimmunol.1403044.
(75.) Formiga F, Meco JF, Pinto X, Jacob J, Moga I, Pujol R. Lipid and lipoprotein levels in premenopausal systemic lupus erythematosus patients. Lupus. 2001;10(5):359-63.
(76.) Yoo WH. Dyslipoproteinemia in patients with active rheumatoid arthritis: effects of disease activity, sex, and menopausal status on lipid profiles. J Rheumatol. 2004 Sep;31(9):1746-53.
(77.) van Leuven SI, Hezemans R, Levels JH, Snoek S, Stokkers PC, Hovingh GK, et al. Enhanced atherogenesis and altered high density lipoprotein in patients with Crohn’s disease. J Lipid Res. 2007 Dec;48(12):2640-6. DOI10.1194/jlr.M700176-JLR200.
(78.) Cui Y, Blumenthal RS, Flaws JA, Whiteman MK, Langenberg P, Bachorik PS, et al. Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med. 2001 Jun;161(11):1413-9.
(79.) Shor R, Wainstein J, Oz D, Boaz M, Matas Z, Fux A, et al. Low HDL levels and the risk of death, sepsis and malignancy. Clin Res Cardiol. 2008 Apr;97(4):227-33. DOI 10.1007/s00392-007-0611-z.
(80.) McMahon M, Grossman J, FitzGerald J, Dahlin-Lee E, Wallace DJ, Thong BY, et al. Proinflammatory highdensity lipoprotein as a biomarker for atherosclerosis in patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum. 2006 Aug;54(8):2541-9. DOI 10.1002/art.21976.
(81.) Peters MJ, van Halm VP, Nurmohamed MT, Damoiseaux J, Tervaert JW, Twisk JW, et al. Relations between autoantibodies against oxidized low-density lipoprotein, inflammation, subclinical atherosclerosis, and cardiovascular disease in rheumatoid arthritis. J Rheumatol. 2008 Aug;35(8):1495-9.
(82.) McMahon M, Grossman J, Skaggs B, Fitzgerald J, Sahakian L, Ragavendra N, et al. Dysfunctional proinflammatory high-density lipoproteins confer increased risk of atherosclerosis in women with systemic lupus erythematosus. Arthritis Rheum. 2009 Aug;60(8):2428-37. DOI 10.1002/art.24677.
(83.) Holven KB, Aukrust P, Retterstøl K, Otterdal K, Bjerkeli V, Ose L, et al. The antiatherogenic function of HDL is impaired in hyperhomocysteinemic subjects. J Nutr. 2008 Nov;138(11):2070-5. DOI 10.3945/jn.108.090704.
(84.) Charakida M, Besler C, Batuca JR, Sangle S, Marques S, Sousa M, et al. Vascular abnormalities, paraoxonase activity, and dysfunctional HDL in primary antiphospholipid syndrome. JAMA. 2009 Sep;302(11):1210-7. DOI 10.1001/jama.2009.1346.
(85.) Vergeer M, Boekholdt SM, Sandhu MS, Ricketts SL, Wareham NJ, Brown MJ, et al. Genetic variation at the phospholipid transfer protein locus affects its activity and high-density lipoprotein size and is a novel marker of cardiovascular disease susceptibility. Circulation. 2010 Aug;122(5):470-7. DOI 10.1161/CIRCULATIONAHA.109.912519.
(86.) Brunham LR, Kang MH, Van Karnebeek C, Sadananda SN, Collins JA, Zhang LH, et al. Clinical, Biochemical, and Molecular Characterization of Novel Mutations in ABCA1 in Families with Tangier Disease. JIMD Rep. 2015;18:51-62. DOI 10.1007/8904_2014_348.
(87.) Mabuchi H, Nohara A, Inazu A. Cholesteryl ester transfer protein (CETP) deficiency and CETP inhibitors. Mol Cells. 2014 Nov;37(11):777-84. DOI 10.14348/molcells.2014.0265.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2017 Iatreia

Esta obra está bajo una licencia internacional Creative Commons Atribución-CompartirIgual 4.0.
Los artículos publicados en la revista están disponibles para ser utilizados bajo la licencia Creative Commons, específicamente son de Reconocimiento-NoComercial-CompartirIgual 4.0 Internacional.
Los trabajos enviados deben ser inéditos y suministrados exclusivamente a la Revista; se exige al autor que envía sus contribuciones presentar los formatos: presentación de artículo y responsabilidad de autoría completamente diligenciados.