Rickettsia spp. infection of the group of spotted fevers in febrile patients of the Urabá Antioquia, Colombia
DOI:
https://doi.org/10.17533/udea.iatreia.15Keywords:
acari, fever of unknown origin, fluorescent antibody technique, indirect, rickettsiaceae infections, zoonosesAbstract
Objective: Determine the frequency of infection and disease by Rickettsia spp. of the spotted fever group in febrile patients from Urabá Antioquia attended by hospital centers of the region.
Methods: Patients from nine health institutions of the Urabá region were included in the study. These patients received a survey with questions about their clinical and socio-demographic variables. Eighty-nine acute- phase serum samples, and 60 convalescent serum samples, were obtained from these patients, and each sample was tested (IgG) by Indirect Immunofluoerscence Assay (IIFA) using a dilution of 1:64 against R. rickettsii. Furtherly, positive sera were tittered by two-fold serial dilutions using the same antigen.
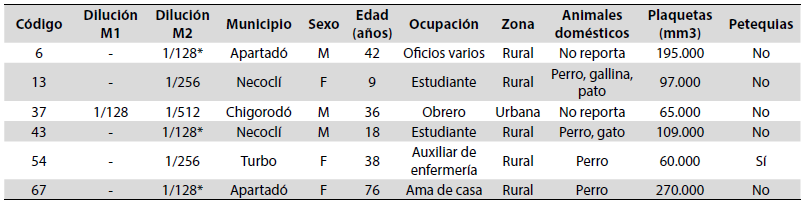
Results: Patients showed symptoms such as fever, headache, jaundice, myalgias, nausea, abdominal pain, petechiae, thrombocytopenia and vomiting. Most of these patients came from rural areas (55,1 %). Seropositivity was obtained in 40,4 % patients with titers between 64-512, a 33,7 % with previous infection and the disease was found in 6 patients (6,7 %). Patients with seroconversion, or a fourlfold rise antibody titer between acute and convalescent samples, came from the municipalities of Apartadó (n = 2), Chigorodó (n = 1), Necoclí (n = 2) and Turbo (n = 1), and the most relevant clinical finding was thrombocytopenia in four of the patients.
Conclusions: This study demonstrated that infection and rickettsial disease continues being active in the Urabá region. This situation represents a warning for the health authorities of the region and suggests them to provide appropriate treatment to avoid deaths or sequelae derived from this type of infections.
Downloads
References
(1.) Gillespie JJ, Williams K, Shukla M, Snyder EE, Nordberg EK, Ceraul SM, et al. Rickettsia phylogenomics: unwinding the intricacies of obligate intracellular life. PLoS One. 2008;3(4): e2018. DOI 10.1371/journal.pone.0002018.
(2.) Gómez Sánchez MM, Gómez Sánchez MC. Rickettsiosis: fiebre botonosa mediterránea. Medicina Integral. 2001; 38(3): 110-15.
(3.) Sahni SK, Narra HP, Sahni A, Walker DH. Recent molecular insights into rickettsial pathogenesis and immunity. Future Microbiol. 2013; 8(10): 1265-88. DOI 10.2217/fmb.13.102.
(4.) Szabó PJ, Pinter A, Labruna, MB. Ecology, biology and distribution of spotted-fever tick vectors in Brazil. Front Cell Infect Microbiol. 2013; 3, (27). DOI 10.3389/fcimb.2013.00027.
(5.) Parola P, Labruna MB, Raoult D. Tick-borne rickettsioses in America: Unanswered questions and emerging diseases. Curr Infect Dis Rep. 2009; 11(1):40-50. DOI 10.1007/s11908-009-0007-5.
(6.) Álvarez Hernández G, Candia Plata MC, Bolado Martínez E, Delgado de la Mora J, Soto Guzmán A, López Soto LF. Fiebre manchada por Rickettsia rickettsii en las Américas: un problema creciente de salud pública. Rev Univ Ind Santander Salud. 2015;47(3):24359. DOI: 10.18273/revsal.v47n3-2015001.
(7.) Dantas Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007;7(11):724-32. DOI 10.1016/S1473-3099(07)70261-X.
(8.) Patiño Camargo L. Fiebre manchada en Tobia, Colombia. Biomedica. 2006; 26(2):178-93.
(9.) Acosta J, Urquijo L, Díaz A, Sepúlveda M, Mantilla G, Heredia D, et al. Brote de rickettsiosis en Necoclí, Antioquia. IQEN. 2006; 11(12):177-86.
(10.) Hidalgo M, Lizarazo D, Ovalle MV, Castañeda E, Heredia D, Zambrano P, et al. Brote de rickettsiosis en Los Córdobas, departamento de Córdoba. IQEN. 2007; 12(24):371-78.
(11.) Pacheco O, Giraldo R, Martínez M, Hidalgo M, Galeano A, Echeverri I, et al. Estudio de brote febril hemorrágico en el corregimiento de Alto de Mulatos - Distrito Especial Portuario de Turbo, Antioquia. IQEN. 2008; 13(10):145-60.
(12.) Miranda AM, Flórez S, Mattar S. Alta seroprevalencia de rickettsiosis en trabajadores del campo en el municipio de Ciénaga de Oro, Córdoba. IQEN. 2002; 7:72-5.
(13.) Hidalgo M, Orejuela L, Fuya P, Carrillo P, Hernández J, Parra E, et al. Rocky Mountain Spotted Fever, Colombia. Emerg Infect Dis. 2007; 13(7):1058-60. DOI 10.3201/eid1307.060537.
(14. ) Acevedo LY, Londoño A, Paternina L, Montes C, Pájaro D, Jaramillo K, et al. Descripción de un nuevo foco de fiebre manchada de las montañas rocosas en el municipio de Uramita, departamento de Antioquia, Colombia. Rev Biomed. 2015; 26(1):113-14.
(15.) Gómez Quintero CH, Faccini Martínez AA, Botero García CA, Lozano M, Sánchez Lerma L, Miranda J, et al. Probable case of spotted fever group rickettsial infection in a new-suspected endemic area, Colombia. J Infect Public Health. 2017; 10(3):353-56. DOI 10.1016/j.jiph.2016.08.012.
(16.) Colombia. Ministerio de Salud y Protección Social, Organización Panamericana de la Salud. Propuesta de abordaje sindrómico de zoonosis con potencial epidémico [internet]. [consultado 2017 oct 2006]. 2012. Disponible en: https://bit.ly/2XbuiT9
(17.) Newhouse VF, Shepard CC, Redus MD, Tzianabos T, McDade JE. A comparison of the complement fixation, indirect fluorescent antibody, and microagglutination tests for the serological diagnosis of rickettsial diseases. Am J Trop Med Hyg. 1979; 28(2):387–95.
(18.) Clements ML, Dumler JS, Fiset P, Wissemant CL Jr, Snyder MJ, Levine MM. Serodiagnosis of Rocky Mountain spotted fever: comparison of IgM and IgG enzyme-linked immunosorbent assays and indirect fluorescent antibody test. J Infect Dis. 1983; 148(5):876–80.
(19.) Philip RN, Casper EA, MacCormack JN, Sexton D, Thomas LA, Anacker RL, et al. A comparison of serologic methods for diagnosis of Rocky Mountain spotted fever. Am J Epidemiol, 1977; 105(1):56–67.
(20.) Londoño AF, Acevedo LY, Marín D, Contreras V, Díaz FJ, Valbuena G, et al. Human prevalence of the spotted fever group (SFG) rickettsiae in endemic zones of Northwestern Colombia. Ticks Tick-borne Dis. 2017; 8(4):477-82. DOI 10.1016/j.ttbdis.2017.02.006.
(21.) Oteo JA, Nava S, Sousa R, Mattar S, Venzal JM, Abarca K, et al. Guías Latinoamericanas de la RIICER para el diagnóstico de las rickettsiosis transmitidas por garrapatas. Rev Chilena Infectol. 2014; 31(1):54-65. DOI org/10.4067/S0716-10182014000100009.
(22.) Portillo A, de Sousa R, Santibanez S, Duarte A, Edouard S, Fonseca, et al. Guidelines for the Detection of Rickettsia spp. Vector Borne Zoonotic Dis. 2017; 17(1):23-32. DOI 10.1089/vbz.2016.1966.
(23.) Díaz JS, Cataño JC. Fiebre manchada de las montañas rocosas: ni tan manchada ni tan montañosa como pensábamos. Infect. 2010; 14(4):264-76 DOI 10.1016/S0123-9392(10)70120-X.
(24.) Labruna MB, Mattar S, Navas S, Bermudez S, Venzal JM, Dols G, et al. Rickettsiosis en América Latina, el Caribe, España y Portugal. Rev.MVZ Córdoba. 2011; 16(2):2435-57.
(25.) Quintero Vélez JC, Londoño AF, Díaz FJ, Agudelo Flórez P, Arboleda M, Rodas JD. Ecoepidemiología de la infección por rickettsias en roedores, ectoparásitos y humanos en el noroeste de Antioquia, Colombia. Biomédica. 2013; 33(1):38-51. DOI 10.7705/biomedica.v33i0.735.
(26.) Padmanabha H, Hidalgo M, Valbuena G, Castañeda E, Galeano A, Puerta H, et al. Geographic variation in risk factors for SFG rickettsial and leptospiral exposure in Colombia. Vector Borne Zoonotic Dis. 2009; 9(5):483-90. DOI 10.1089/vbz.2008.0092.
(27.) Arroyave E, Londoño AF, Quintero JC, Agudelo Flórez P, Arboleda M, Díaz FJ, et al. Etiología y caracterización epidemiológica del síndrome febril no palúdico en tres municipios del Urabá antioqueño, Colombia. Biomedica. 2013; 33(1):99-107. DOI 10.7705/biomedica.v33i0.734.
(28.) Londoño AF, Acevedo LY, Marín D, Contreras V, Díaz FJ, Valbuena G, et al. Wild and domestic animals likely involved in rickettsial endemic zones of Northwestern Colombia. Ticks Tick Borne Dis. 2017; 8(6):887-94. DOI 10.1016/j.ttbdis.2017.07.007.
(29.) Arguello AP, Hun L, Rivera P, Taylor L. A fatal urban case of Rocky Mountain spotted fever presenting an eschar in San Jose, Costa Rica. Am J Trop Med
Hyg. 2012; 87(2):345-8. DOI 10.4269/ajtmh.2012.12-0153.
(30.) Estripeaut D, Aramburu MG, Saez-Llorens X, Thompson HA, Dasch GA,
Paddock CD, et al. Rocky Mountain spotted fever, Panama. Emerg Infect Dis.
; 13(11):1763-65. DOI 10.3201/eid1311.070931.
(31.) Pinter A, França AC, de Souza CE, Sabbo C, Mendes do Nascimento EM, Fabiana Pereira dos Santos C, et al. Febre maculosa brasileira. BEPA. 2011; 8(1):3-31.
(32.) Paddock CD, Fernandez S, Echenique GA, Sumner JW, Reeves WK, Zaki SR, et al. Rocky Mountain spotted fever in Argentina. Am J Trop Med Hyg. 2008; 78(4):687-92.
(33.) Hidalgo M, Faccini Martínez AA, Valbuena G. Rickettsiosis transmitidas por garrapatas en las Américas: avances clínicos y epidemiológicos, y retos en el diagnóstico. Biomedica. 2013; 33(1):161-78. DOI 10.7705 /biomedica.v33i0.1466.
(34.) Abarca K, Oteo JA. Aproximación clínica y principales rickettsiosis transmitidas por garrapatas presentes en Latinoamérica. Rev. chil. infectol. 2014; 31(5): 569-76. DOI 10.4067/S0716-10182014000500009.
(35.) Quintero Vélez JC, Paternina LE, Uribe A, Muskus C, Hidalgo M, Gil J, et al. Eco-epidemiological analysis of rickettsial seropositivity in rural areas of Colombia: A multilevel approach. PLoS Negl Trop Dis. 2017; 11(9):e0005892. DOI 10.1371/journal.pntd.0005892.
(36.) Pinter A, Horta MC, Pacheco RC, Moraes-Filho J, Labruna MB. Serosurvey of Rickettsia spp. in dogs and humans from an endemic area for Brazilian spotted fever in the State of São Paulo, Brazil. Cad Saude Publica. 2008; 24(2):247-52. DOI 10.1590/S0102-311X200800020000.
(37.) Sangioni LA, Horta MC, Vianna MC, Gennari SM, Soares RM, Labruna MB, et al. Rickettsial Infection in Animals and Brazilian Spotted Fever Endemicity. Emerg Infect Dis. 2005; 11(2):265-70. DOI 10.3201/eid1102.040656.
Published
How to Cite
Issue
Section
License
Copyright (c) 2019 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.