Investigación de la eficacia y criterios de aprobación de los tratamientos con medicamentos para pacientes con cáncer: una revisión
DOI:
https://doi.org/10.17533/udea.iatreia.v31n3a06Palabras clave:
aprobación de drogas, evaluación de medicamentos, neoplasias, oncología médica, terapéuticaResumen
Los diversos trastornos malignos de los tejidos humanos afectan a una gran proporción de personas de Colombia y el mundo, lo que ha llevado al incremento de los tratamientos farmacológicos para estas enfermedades, sin que se tenga claro el real beneficio para los pacientes que los reciben. Además, se tienen dudas sobre la calidad de la evidencia en la que se basan las instituciones que avalan los tratamientos anti-cáncer con medicamentos, como son la Food and Drug Administration (FDA) y la European Medicines Agency (EMA). Este trabajo tuvo como objetivo conocer cómo se realizan los estudios de eficacia y la forma en que se aprueban los tratamientos con medicamentos que se ofrecen a las personas con cáncer; se realizó una revisión narrativa, que se basó en la formulación de preguntas que guiaron el desarrollo de los temas que se incluyeron en ella. Se hizo la búsqueda de la información en Pubmed de una forma estructurada, no sistemática. Se incluyeron artículos publicados en inglés y español, sin restricción por fecha de publicación.
Descargas
Citas
(1.) Venook AP, Tabernero J. Progression-free survival: helpful biomarker or clinically meaningless end point? J Clin Oncol. 2015 Jan;33(1):4-6. DOI 10.1200/JCO.2014.57.9557.
(2.) Guidance for Industry Clinical Trial Endpoints for the Approval of Cancer Drugs and Biologics. U.S. Department of Health and Human Services. Food and Drug Administration Center for Drug Evaluation and Research (CDER). Center for Biologics Evaluation and Research (CBER). 2007. (consultado el 20 de agosto de 2017) Disponible en: https://www.fda.gov/downloads/Drugs/Guidances/ucm071590.pdf
(3.) Peppercorn JM, Smith TJ, Helft PR, Debono DJ, Berry SR, Wollins DS, et al. American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol. 2011 Feb;29(6):755-60. DOI 10.1200/JCO.2010.33.1744.
(4.) Ellis LM, Bernstein DS, Voest EE, Berlin JD, Sargent D, Cortazar P, et al. American Society of Clinical Oncology perspective: Raising the bar for clinical trials by defining clinically meaningful outcomes. J Clin Oncol. 2014 Apr;32(12):1277-80. DOI 10.1200/JCO.2013.53.8009.
(5.) Davis C, Naci H, Gurpinar E, Poplavska E, Pinto A, Aggarwal A. Availability of evidence of benefits on overall survival and quality of life of cancer drugs approved by European Medicines Agency: retrospective cohort study of drug approvals 2009-13. BMJ. 2017 Oct;359:j4530. DOI 10.1136/bmj.j4530.
(6.) Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015 Jan-Feb;65(1):5-29. DOI 10.3322/caac.21254.
(7.) Wise PH. Cancer drugs, survival, and ethics. BMJ. 2016;355:i5792. DOI 10.1136/bmj.i5792.
(8.) Morgan G, Ward R, Barton M. The contribution of cytotoxic chemotherapy to 5-year survival in adult malignancies. Clin Oncol (R Coll Radiol). 2004 Dec;16(8):549-60.
(9.) Fojo T, Mailankody S, Lo A. Unintended consequences of expensive cancer therapeutics—the pursuit of marginal indications and a me-too mentality that stifles innovation and creativity: the John Conley Lecture. JAMA Otolaryngol Head Neck Surg. 2014 Dec;140(12):1225-36. DOI 10.1001/jamaoto.2014.1570.
(10.) Apolone G, Joppi R, Bertele’ V, Garattini S. Ten years of marketing approvals of anticancer drugs in Europe: regulatory policy and guidance documents need to find a balance between different pressures. Br J Cancer. 2005 Sep 5;93(5):504-9.
(11.) Hiom SC. Diagnosing cancer earlier: reviewing the evidence for improving cancer survival. Br J Cancer. 2015 Mar;112 Suppl 1:S1-5. DOI 10.1038/bjc.2015.23.
(12.) Bauman JR, Temel JS. The integration of early palliative care with oncology care: the time has come for a new tradition. J Natl Compr Canc Netw. 2014 Dec;12(12):1763-71; quiz 1771.
(13.) Storme G, Dhaese S, Corens D, De Ridder M. The cost of cancer care is not related to its outcomes. Ecancermedicalscience. 2016 Oct;10:687.
(14.) Grössmann N, Del Paggio JC, Wolf S, Sullivan R, Booth CM, Rosian K, et al. Five years of EMA-approved systemic cancer therapies for solid tumours-a comparison of two thresholds for meaningful clinical benefit. Eur J Cancer. 2017 Sep;82:66-71. DOI 10.1016/j.ejca.2017.05.029.
(15.) Genentech. Oncology Endpoints in a Changing Landscape. Am J Manag Care [Internet]. 2016 Jan [consultado Nov 2017]. Disponible en: https://www.managedcaremag.com/sites/default/files/graphics/OncoEndpoints_MC.pdf
(16.) Fiteni F, Westeel V, Pivot X, Borg C, Vernerey D, Bonnetain F. Endpoints in cancer clinical trials. J Visc Surg. 2014 Feb;151(1):17-22. DOI 10.1016/j.jviscsurg.2013.10.001.
(17.) McKee AE, Farrell AT, Pazdur R, Woodcock J. The role of the U.S. Food and Drug Administration review process: clinical trial endpoints in oncology. Oncologist. 2010;15 Suppl 1:13-8. DOI 10.1634/theoncologist.2010-S1-13.
(18.) Booth CM, Eisenhauer EA. Progression-free survival: meaningful or simply measurable? J Clin Oncol. 2012 Apr;30(10):1030-3. DOI 10.1200/JCO.2011.38.7571.
(19.) Gaddipati H, Liu K, Pariser A, Pazdur R. Rare cancer trial design: lessons from FDA approvals. Clin Cancer Res. 2012 Oct;18(19):5172-8. DOI 10.1158/1078-0432.CCR-12-1135.
(20.) Wilson MK, Karakasis K, Oza AM. Outcomes and endpoints in trials of cancer treatment: the past, present, and future. Lancet Oncol. 2015 Jan;16(1):e32-42. DOI 10.1016/S1470-2045(14)70375-4.
(21.) Prasad V, Kim C, Burotto M, Vandross A. The Strength of Association Between Surrogate End Points and Survival in Oncology: A Systematic Review of Trial-Level Meta-analyses. JAMA Intern Med. 2015 Aug;175(8):1389-98. DOI 10.1001/jamainternmed.2015.2829.
(22.) Kim C, Prasad V. Strength of Validation for Surrogate End Points Used in the US Food and Drug Administration’s Approval of Oncology Drugs. Mayo Clin Proc. 2016 May. pii: S0025-6196(16)00125-7. DOI 10.1016/j.mayocp.2016.02.012.
(23.) Driscoll JJ, Rixe O. Overall survival: still the gold standard: why overall survival remains the definitive end point in cancer clinical trials. Cancer J. 2009 Sep-Oct;15(5):401-5. DOI 10.1097/PPO.0b013e3181bdc2e0.
(24.) Nishino M, Giobbie-Hurder A, Gargano M, Suda M, Ramaiya NH, Hodi FS. Developing a common language for tumor response to immunotherapy: immune-related response criteria using unidimensional measurements. Clin Cancer Res. 2013 Jul;19(14):3936-43. DOI 10.1158/1078-0432.CCR-13-0895.
(25.) Hoos A, Eggermont AM, Janetzki S, Hodi FS, Ibrahim R, Anderson A, et al. Improved endpoints for cancer immunotherapy trials. J Natl Cancer Inst. 2010 Sep;102(18):1388-97. DOI 10.1093/jnci/djq310.
(26.) Darrow JJ, Avorn J, Kesselheim AS. New FDA breakthrough-drug category--implications for patients. N Engl J Med. 2014 Mar;370(13):1252-8. DOI 10.1056/NEJMhle1311493. Erratum in: N Engl J Med. 2014 Jul;371(1):94.
(27.) Richey EA, Lyons EA, Nebeker JR, Shankaran V, Mc-Koy JM, Luu TH, et al. Accelerated approval of cancer drugs: improved access to therapeutic breakthroughs or early release of unsafe and ineffective drugs? J Clin Oncol. 2009 Sep;27(26):4398-405. DOI 10.1200/JCO.2008.21.1961.
(28.) Senderowicz AM, Pfaff O. Similarities and differences in the oncology drug approval process between FDA and European Union with emphasis on in vitro companion diagnostics. Clin Cancer Res. 2014 Mar;20(6):1445-52. DOI 10.1158/1078-0432.CCR-13-1761.
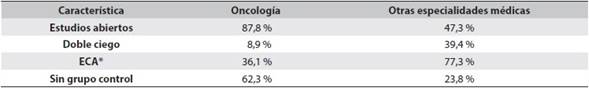
(29.) Tafuri G, Stolk P, Trotta F, Putzeist M, Leufkens HG, Laing RO, et al. How do the EMA and FDA decide which anticancer drugs make it to the market? A comparative qualitative study on decision makers’ views. Ann Oncol. 2014 Jan;25(1):265-9. DOI 10.1093/annonc/mdt512.
(30.) Pignatti F, Gravanis I, Herold R, Vamvakas S, Jonsson B, Marty M. The European Medicines Agency: an overview of its mission, responsibilities, and recent initiatives in cancer drug regulation. Clin Cancer Res. 2011 Aug;17(16):5220-5. DOI 10.1158/1078-0432.CCR-11-0623.
(31.) Hartmann M, Mayer-Nicolai C, Pfaff O. Approval probabilities and regulatory review patterns for anticancer drugs in the European Union. Crit Rev Oncol Hematol. 2013 Aug;87(2):112-21. DOI 10.1016/j.critrevonc.2013.01.004.
(32.) Sridhara R, Johnson JR, Justice R, Keegan P, Chakravarty A, Pazdur R. Review of oncology and hematology drug product approvals at the US Food and Drug Administration between July 2005 and December 2007. J Natl Cancer Inst. 2010 Feb;102(4):230-43. DOI 10.1093/jnci/djp515. Erratum in: J Natl Cancer Inst. 2010 Apr;102(8):578-9.
(33.) Johnson JR, Williams G, Pazdur R. End points and United States Food and Drug Administration approval of oncology drugs. J Clin Oncol. 2003 Apr;21(7):1404-11.
(34.) Downing NS, Aminawung JA, Shah ND, Krumholz HM, Ross JS. Clinical trial evidence supporting FDA approval of novel therapeutic agents, 2005-2012. JAMA. 2014 Jan;311(4):368-77. DOI 10.1001/jama.2013.282034.
(35.) Hirsch BR, Califf RM, Cheng SK, Tasneem A, Horton J, Chiswell K, et al. Characteristics of oncology clinical trials: insights from a systematic analysis of Clinical-Trials.gov. JAMA Intern Med. 2013 Jun;173(11):972-9. DOI 10.1001/jamainternmed.2013.627. Erratum in: JAMA Intern Med. 2013 Sep;173(16):1560.
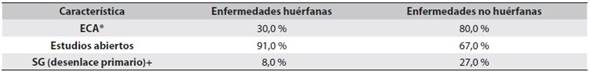
(36.) Kesselheim AS, Myers JA, Avorn J. Characteristics of clinical trials to support approval of orphan vs nonorphan drugs for cancer. JAMA. 2011 Jun;305(22):2320-6. DOI 10.1001/jama.2011.769.
(37.) Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004 Jun;291(22):2720-6.
(38.) Nurgat ZA, Craig W, Campbell NC, Bissett JD, Cassidy J, Nicolson MC. Patient motivations surrounding participation in phase I and phase II clinical trials of cancer chemotherapy. Br J Cancer. 2005 Mar;92(6):1001-5.
(39.) Zapata ML, Jaimes FA. Ronda Clínica y Epidemiológica. Desenlaces sustitutos en investigación médica. Iatreia. 2012 Jul-Sep;25(3):287-93.
(40.) Johnson JR, Ning YM, Farrell A, Justice R, Keegan P, Pazdur R. Accelerated approval of oncology products: the food and drug administration experience. J Natl Cancer Inst. 2011 Apr;103(8):636-44. DOI 10.1093/jnci/djr062.
(41.) Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-90. DOI 10.1634/theoncologist.2012-0279.
(42.) Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012 Oct;367(17):1616-25. DOI 10.1056/NEJMoa1204410.
(43.) Audrey S, Abel J, Blazeby JM, Falk S, Campbell R. What oncologists tell patients about survival benefits of palliative chemotherapy and implications for informed consent: qualitative study. BMJ. 2008 Jul;337:a752.DOI 10.1136/bmj.a752.
(44.) Chan JK, Kiet TK, Monk BJ, Young-Lin N, Blansit K, Kapp DS, et al. Applications for oncologic drugs: a descriptive analysis of the oncologic drugs advisory committee reviews. Oncologist. 2014 Mar;19(3):299-304. DOI 10.1634/theoncologist.2013-0276.
(45.) Wallington M, Saxon EB, Bomb M, Smittenaar R, Wickenden M, McPhail S, et alk. 30-day mortality after systemic anticancer treatment for breast and lung cancer in England: a population-based, observational study. Lancet Oncol. 2016 Sep;17(9):1203-16. DOI 10.1016/S1470-2045(16)30383-7. Erratum in: Lancet Oncol. 2016 Oct;17(10):e420.
(46.) Wright AA, Zhang B, Keating NL, Weeks JC, Prigerson HG. Associations between palliative chemotherapy and adult cancer patients’ end of life care and place of death: prospective cohort study. BMJ. 2014 Mar;348:g1219. DOI 10.1136/bmj.g1219.
(47.) Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000 Fall;3(3):287-300.
(48.) Light DW, Lexchin J. Why do cancer drugs get such an easy ride? BMJ. 2015 Apr;350:h2068. DOI 10.1136/bmj.h2068.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2018 Iatreia

Esta obra está bajo una licencia internacional Creative Commons Atribución-CompartirIgual 4.0.
Los artículos publicados en la revista están disponibles para ser utilizados bajo la licencia Creative Commons, específicamente son de Reconocimiento-NoComercial-CompartirIgual 4.0 Internacional.
Los trabajos enviados deben ser inéditos y suministrados exclusivamente a la Revista; se exige al autor que envía sus contribuciones presentar los formatos: presentación de artículo y responsabilidad de autoría completamente diligenciados.