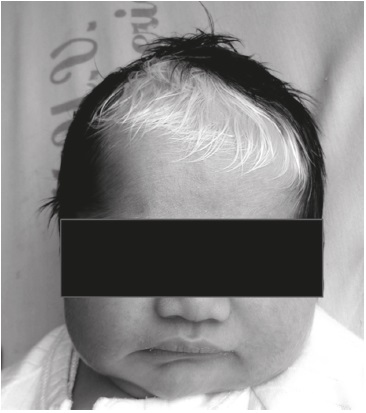
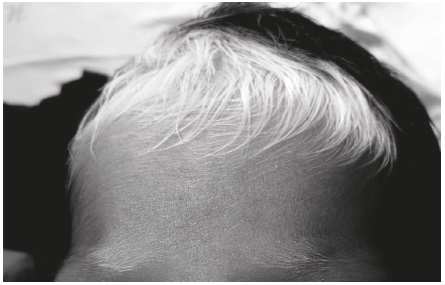
Piebaldism-Moebius and prenatal exposure to misoprostol: a case report
DOI:
https://doi.org/10.17533/udea.iatreia.v29n1a08Keywords:
birth defects, hypopigmentation, Mobius Syndrome, Misoprostol, piebaldism, pregnancyAbstract
Piebaldism is a rare congenital disease with prevalence of 1/100.000, characterized by patchy depigmentation of the skin and the presence of a white forelock. Its course is static and otherwise patients are healthy. It is inherited in an autosomal dominant pattern and is caused by mutations in the gene c-kit, a proto-oncogene involved in the migration, proliferation, differentiation and survival of melanoblasts. On the other hand, Moebius syndrome is a congenital palsy of the VII cranial nerve, which may be associated with involvement of other cranial nerves, or even of other systems. In the United States its frequency has been calculated from 0.002% to 0.0002% of total births. We report the case of a newborn girl with piebaldism and Moebius syndrome associated with prenatal exposure to misoprostol. A search was made about these anomalies and the association between prenatal exposure to misoprostol and congenital anomalies. Piebaldism is a rare genetic disorder. On the other hand, the cause of Moebius syndrome is heterogeneous and not well defined, and it has been associated with prenatal exposure to misoprostol. Our patient had simultaneously two diseases: one purely genetic and the other potentially teratogenic.
Downloads
References
(1.) Sarma N, Chakraborty S, Bhanja DC, Bhattachraya SR. Piebaldism with non-intertriginous freckles: what does it mean? Indian J Dermatol Venereol Leprol. 2014 Mar-Apr;80(2):163-5.
(2.) Spritz RA. Piebaldism, Waardenburg syndrome, and related disorders of melanocyte development. Semin Cutan Med Surg. 1997 Mar;16(1):15-23.
(3.) Thomas I, Kihiczak GG, Fox MD, Janniger CK, Schwartz RA. Piebaldism: an update. Int J Dermatol. 2004 Oct;43(10):716-9.
(4.) Hwang SM, Ahn SK, Lee WS, Yoo MS, Choi EH. Piebaldism-a case report. J Korean Med Sci. 1996 Jun;11(3):285-8.
(5.) Medscape [Internet]. Nueva York: Medscape; 2014[cited 2014 Dec 12]. Palmer CA. Mobius Syndrome. Available from: http://emedicine.medscape.com/article/1180822-overview
(6.) Vargas FR, Schuler-Faccini L, Brunoni D, Kim C, Meloni VF, Sugayama SM, et al. Prenatal exposure to misoprostol and vascular disruption defects: a casecontrol study. Am J Med Genet. 2000 Dec;95(4):302-6.
(7.) da Silva Dal Pizzol T, Knop FP, Mengue SS. Prenatal exposure to misoprostol and congenital anomalies: systematic review and meta-analysis. Reprod Toxicol. 2006 Nov;22(4):666-71.
(8.) Spritz RA. Molecular basis of human piebaldism. J Invest Dermatol. 1994 Nov;103(5 Suppl):137S-140S.
(9.) Hartmann A, Bröcker EB, Becker JC. Hypopigmentary skin disorders: current treatment options and future directions. Drugs. 2004;64(1):89- 107.
(10.) Murakami T, Fukai K, Oiso N, Hosomi N, Kato A, Garganta C, et al. New KIT mutations in patients with piebaldism. J Dermatol Sci. 2004 Jun;35(1):29-33.
(11.) Caballero Moreno LM, Mosquera Sánchez H. Piebaldismo: reporte de un caso y revisión de la literatura. MedUNAB. 2006;9(1):72-5.
(12.) Ward KA, Moss C, Sanders DS. Human piebaldism: relationship between phenotype and site of kit gene mutation. Br J Dermatol. 1995 Jun;132(6):929-35.
(13.) Ezoe K, Holmes SA, Ho L, Bennett CP, Bolognia JL, Brueton L, et al. Novel mutations and deletions of the KIT (steel factor receptor) gene in human piebaldism. Am J Hum Genet. 1995 Jan;56(1):58-66.
(14.) Syrris P, Malik NM, Murday VA, Patton MA, Carter ND, Hughes HE, et al. Three novel mutations of the protooncogene KIT cause human piebaldism. Am J Med Genet. 2000 Nov;95(1):79-81.
(15.) Grichnik JM, Rhodes AR, Sobe AJ. Hypomelanoses and hypermelanoses. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI. Fitzpatrick ́s dermatology in general medicine. 6ª ed. New York: McGraw-Hill; 2003. p. 925-72.
(16.) Njoo MD, Nieuweboer-Krobotova L, Westerhof W. Repigmentation of leucodermic defects in piebaldism by dermabrasion and thin split-thickness skin grafting in combination with minigrafting. Br J Dermatol. 1998 Nov;139(5):829-33.
(17.) Henderson JL. The congenital facial diplegia syndrome: clinical features, pathology and etiology. Brain. 1939 Dec;62(4):381-403.
(18.) Möbius PJ. [Uber angeborene doppelseitige Abducens-Facialis-lähmung]. Munch Med Wochenschr. 1888;35:91-4. German.
(19.) Pérez Aytés A. Síndrome de Moebius. Protoc Diagn Ter Pediatr. 2010;1:80-4.
(20.) Verzijl HT, van der Zwaag B, Cruysberg JR, Padberg GW. Möbius syndrome redefined: a syndrome of rhombencephalic maldevelopment. Neurology. 2003 Aug;61(3):327-33.
(21.) Norman JE, Thong KJ, Baird DT. Uterine contractility and induction of abortion in early pregnancy by misoprostol and mifepristone. Lancet. 1991 Nov;338(8777):1233-6.
(22.) Costa SH. Commercial availability of misoprostol and induced abortion in Brazil. Int J Gynaecol Obstet. 1998 Dec;63 Suppl 1:S131-9.
(23.) Schüler L, Ashton PW, Sanseverino MT. Teratogenicity of misoprostol. Lancet. 1992 Feb;339(8790):437.
(24.) Schüler L, Pastuszak A, Sanseverino TV, Orioli IM, Brunoni D, Ashton-Prolla P, et al. Pregnancy outcome after exposure to misoprostol in Brazil: a prospective, controlled study. Reprod Toxicol. 1999 Mar-Apr;13(2):147-51.
Published
How to Cite
Issue
Section
License
Copyright (c) 2015 Iatreia

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Papers published in the journal are available for use under the Creative Commons license, specifically Attribution-NonCommercial-ShareAlike 4.0 International.
The papers must be unpublished and sent exclusively to the Journal Iatreia; the author uploading the contribution is required to submit two fully completed formats: article submission and authorship responsibility.