Ronda clínica y epidemiológica: club de revistas
DOI:
https://doi.org/10.17533/udea.iatreia.v30n2a13Palabras clave:
alimentación mixta, antibacterianos, combinación trimetoprim y sulfametoxazol, enfermedad pulmonar obstructiva crónica:, espirometría, fiebre, hábito de fumar, hipersensibilidad a los alimentos, lactancia materna, staphylococcus aureus resistente a meticilinaResumen
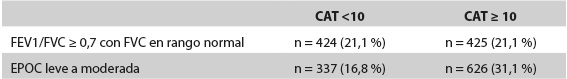
En esta edición de la Ronda Clínica y Epidemiológica analizamos cuatro artículos que consideramos importantes para la práctica clínica. El estudio del grupo SPIROMICS busca replantear la necesidad de la espirometría para el diagnóstico de enfermedad pulmonar obstructiva crónica (EPOC), especialmente en los pacientes con antecedente de tabaquismo que tienen función pulmonar normal, pero desarrollan desenlaces de enfermedad pulmonar crónica. Borja-Gómez y colaboradores, por otro lado, validan un enfoque sistemático para descartar infecciones bacterianas invasivas en niños febriles menores de 3 meses. El estudio de Talan y colaboradores estima la utilidad del tratamiento antibiótico con trimetoprim-sulfametoxazol, adicional al drenaje quirúrgico, como una estrategia para mejorar la curación de abscesos en piel en una población con alta prevalencia de Staphylococcus aureus resistente a meticilina (MRSA). Por último, el estudio del grupo EAT que analiza la introducción de alimentos alergénicos en lactantes a partir de los 3 meses, como una estrategia para proteger contra el desarrollo de reacciones alérgicas alimentarias posteriores.
Descargas
Citas
(1.) Couper D, LaVange LM, Han M, Barr RG, Bleecker E, Hoffman EA, et al. Design of the Subpopulations and Intermediate Outcomes in COPD Study (SPIRO- MICS). Thorax. 2014 May;69(5):491-4. DOI 10.1136/thoraxjnl-2013-203897.
(2.) Woodruff PG, Barr RG, Bleecker E, Christenson SA, Couper D, Curtis JL, et al. Clinical Significance of Symptoms in Smokers with Preserved Pulmonary Function. N Engl J Med. 2016 May;374(19):1811-21. DOI 10.1056/NEJMoa1505971.
(3.) Global Initiative for Chronic Obstructive Lung Disea- se [Internet]. Barcelona: GOLD; 2016 [cited 2016 Nov 18]. Global Strategy for Diagnosis, Management, and Prevention of COPD – 2016. Available from: http://goldcopd.org/global-strategy-diagnosis-manage- ment-prevention-copd-2016/
(4.) Baker MD, Bell LM, Avner JR. Outpatient management without antibiotics of fever in selected infants. N Engl J Med. 1993 Nov;329(20):1437-41.
(5.) Jaskiewicz JA, McCarthy CA, Richardson AC, White KC, Fisher DJ, Dagan R, et al. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Febrile Infant Collaborative Study Group. Pediatrics. 1994 Sep;94(3):390-6.
(6.) Baskin MN, O’Rourke EJ, Fleisher GR. Outpatient treatment of febrile infants 28 to 89 days of age with intramuscular administration of ceftriaxone. J Pediatr. 1992 Jan;120(1):22-7.
(7.) Nield LS, Kamat D. Fiebre sin Foco. En: Kliegman RM, Stanton BF, St. Geme JW, Schor NF. Nelson Tratado de Pediatría. 20a ed. España: Elsevier; 2016. p. 1336-46.
(8.) Agudelo M, Rodriguez CA, Vesga O. Trimetoprim-Sulfametoxazol. En: Vesga O, Vélez LA, Leiderman EW, Restrepo AM. Enfermedades Infecciosas de Homo Sapiens. Medellín: CIB; 2015. p. 523-38.
(9.) Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011 Feb;52(3):285-92. DOI 10.1093/cid/cir034.
(10.) Duong M, Markwell S, Peter J, Barenkamp S. Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient. Ann Emerg Med. 2010 May;55(5):401-7. DOI 10.1016/j.annemergmed.2009.03.014.
(11.) Schmitz GR, Bruner D, Pitotti R, Olderog C, Livengood T, Williams J, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplica- ted skin abscesses in patients at risk for community- associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med. 2010 Sep;56(3):283-7. DOI 10.1016/j.annemergmed.2010.03.002. Erratum in: Ann Emerg Med. 2010 Nov;56(5):588.
(12.) Valderrama SL, Gualtero S, Rodriguez J, Osorio J, Alvarez CA, Gil F. Risk Factors Associated with Methicillin-Resistant Staphylococcus aureus (MRSA) Complicated Skin and Soft Tissue Infection (CSSTIs) in Colombia. In: ID Week. Clinical Infectious Diseases: Bone and Joint, Skin and Soft Tissue [Internet]. New Orleans: ID Week; 2016 [cited 2016 Nov 27]. Availa- ble from: https://idsa.confex.com/idsa/2016/webpro-gram/Paper60161.html
(13.) Departamento de Salud y Servicios Humanos de los Estados Unidos Oficina para la Salud de la Mujer. ¿Cuándo debería empezar a amamantar? En: Guía fácil para la lactancia [Internet]. Washington, DC: DHHS; 2016. p. 5-7 [consultado 2016 Nov 28]. Disponible en: https://www.in.gov/icw/files/lactancia.pdf
(14.) Organización mundial de la salud [Internet]. Ginebra, Suiza: OMS; 2017 [consultado 2016 Nov 28]. Inicio temprano de la lactancia materna. Disponible en: http://www.who.int/elena/titles/early_breastfeeding/es/
(15.) Colombia. Ministerio la protección social; Organización Panamericana de la Salud; Atención Integral a las Enfermedades Prevalentes de la infancia. Guía para la atención y la consejería de la niñez en la familia [Internet]. Bogotá: OPS; 2010 [consultado 2016 Nov 28]. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/GUIA-PA-RA-LA-ATENCION-DE-LA-NINEZ-EN-LA-FAMILIA.pdf
(16.) Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015 Feb;372(9):803-13. DOI 10.1056/NEJMoa1414850. Erratum in: N Engl J Med. 2016 Jul;375(4):398.
(17.) Du Toit G, Katz Y, Sasieni P, Mesher D, Maleki SJ, Fisher HR, et al. Early consumption of peanuts in infancy is associated with a low prevalence of peanut allergy. J Allergy Clin Immunol. 2008 Nov;122(5):984-91. DOI 10.1016/j.jaci.2008.08.039.
(18.) Koplin JJ, Osborne NJ, Wake M, Martin PE, Gurrin LC, Robinson MN, et al. Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol. 2010 Oct;126(4):807- 13. DOI 10.1016/j.jaci.2010.07.028.
(19.) Katz Y, Rajuan N, Goldberg MR, Eisenberg E, Heyman E, Cohen A, et al. Early exposure to cow’s milk protein is protective against IgE-mediated cow’s milk protein allergy. J Allergy Clin Immunol. 2010 Jul;126(1):77-82. e1. DOI 10.1016/j.jaci.2010.04.020.
(20.) Perkin MR, Logan K, Tseng A, Raji B, Ayis S, Peacock J, et al. Randomized Trial of Introduction of Allergenic Foods in Breast-Fed Infants. N Engl J Med. 2016 May;374(18):1733-43. DOI 10.1056/NEJMoa1514210.
(21.) Chafen JJ, Newberry SJ, Riedl MA, Bravata DM, Maglione M, Suttorp MJ, et al. Diagnosing and managing common food allergies: a systematic review. JAMA. 2010 May;303(18):1848-56. DOI 10.1001/jama.2010.582.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2017 Iatreia

Esta obra está bajo una licencia internacional Creative Commons Atribución-CompartirIgual 4.0.
Los artículos publicados en la revista están disponibles para ser utilizados bajo la licencia Creative Commons, específicamente son de Reconocimiento-NoComercial-CompartirIgual 4.0 Internacional.
Los trabajos enviados deben ser inéditos y suministrados exclusivamente a la Revista; se exige al autor que envía sus contribuciones presentar los formatos: presentación de artículo y responsabilidad de autoría completamente diligenciados.